By: Ranier Simons, ADAP Blog Guest Contributor
Even though the COVID-19 pandemic emergency designation is no longer in effect, COVID-19 remains a very present public health issue. Research continues to unearth and examine its mechanisms and effects on the body. Understanding COVID-19 is vital for people living with HIV (PLWH) because co-infection with HIV has different consequences than for those who are HIV-negative. Studies continue to reveal the results of the interactions of HIV and COVID-19 and the realities of long Covid.
 |
| Photo Source: HIV.gov |
A significant difference discovered regarding HIV and COVID-19 is that PLWH are at a higher risk of being reinfected with COVID-19 after an initial bout. The Centers for Disease Control & Prevention (CDC) and the Chicago Department of Public Health studied 453,000 Chicago residents who contracted COVID-19. They found that 5.2% of HIV-negative people experienced reinfection, while the reinfection rate of PLWH was 6.7%.[1] Additionally, data showed that PLWH had higher primary vaccination plus booster rates than the general population at 31.8% and 27%, respectively.[1] This supports the hypothesis that HIV infection is a reinfection risk causal factor.
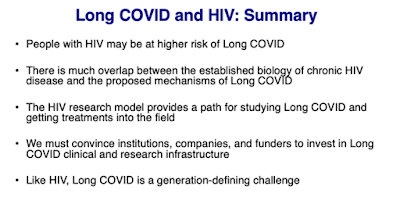
Increased risk of developing long Covid is another reality of the intersection of HIV and COVID-19. Long Covid is defined as a range of over 200 symptoms that linger or appear after an acute episode of Covid-19.[3,6] This wide range of symptoms can last months or years. Frequently reported symptoms of long covid include cognitive impairment (brain fog), incessant fatigue, loss of smell, muscle pain, shortness of breath, post-exertional malaise (inability to recover after exercise), and postural orthostatic tachycardia syndrome (POTS).[2,3,4] POTS is a relatively new term to describe a condition that has previously gone without a name. It is an issue with the autonomic nervous system that can cause fainting, rapid heartbeat, and dizziness.[5] Additionally, research presented at the 2023 Conference on Retroviruses and Opportunistic Infections (CROI), shows that not only are PLWH more likely to have persistent long Covid symptoms but have an increased risk of developing new diseases such as diabetes, heart disease, and cancer.[2,7]
 |
| Photo Source: Michael Peluso, MD | IAS 2023 |
Some possible causes of long Covid symptoms are inflammation, persistent SARS-CoV-2 infection, reactivation of existing pathogens, immune responses that don’t return to normal after acute infection, and "leaky gut" condition.[2] HIV is already known to cause microbial translocation, known as leaky gut. This means weakened intestinal wall permeability allows bacteria and their toxins into the bloodstream, causing disease. Since studies are showing that long Covid symptoms may be due to the SARS-CoV-2 virus causing loss of gut wall integrity, having HIV compounds that condition.[3] Research has also proven that PLWH have higher levels of chronic inflammation, which could compound the inflammation caused by Sars-CoV-2 that raises risks of long Covid.[3] PLWH have increased susceptibility to vascular disease and endothelial dysfunction.[8] This can worsen long Covid related clotting and heart problems.[2,8]
Continuing research is necessary to investigate all the nuances of HIV and Sars-CoV-2 infection. Most notably, it is essential to delineate how long Covid amidst PLWH differs from the general population. At present, it is imperative that PLWH continue to follow medical guidelines concerning staying up to date with COVID-19 vaccinations and remaining consistent in treating comorbid conditions. Research shows that vaccination does reduce the severity of long Covid symptoms, even though it is true that PLWH may experience long Covid at a higher rate than the general population.[2,3] Additionally, it is crucial that PLWH are included in clinical trials investigating treatments for long Covid symptoms.
[1] Kekatos.M. *2923, October 18). People with HIV at higher risk of COVID reinfection: CDC. Retrieved from https://abcnews.go.com/Health/people-hiv-higher-risk-covid-reinfection-cdc/story?id=104035803
[2] Highleyman, L. (2024, January 17). Are people with HIV at greater risk for long COVID. Retrieved from https://www.poz.com/article/people-hiv-greater-risk-long-covid
[3] Alcorn, K. (@023, June 13).More evidence that long COVID is more common in people with HIV. Retrieved from https://www.aidsmap.com/news/jun-2023/more-evidence-long-covid-more-common-people-hiv
[4] Davis, H., Assaf, G., McCorkell, L., Wei, H., Low, R., Re’em, Y., Redfield, S., Austin, J. P., & Akrami, A. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38, 101019. https://doi.org/10.1016/j.eclinm.2021.101019
[5] Morris, A. (2023, February 23). A condition called POTS rose after covid, but patients can’t find care. Retrieved from https://www.washingtonpost.com/wellness/2023/02/27/pots-heart-fainting-long-covid/
[6] Davis, H., Assaf, G., McCorkell, L., Wei, H., Low, R., Re’em, Y., Redfield, S., Austin, J. P., & Akrami, A. (2021b). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38, 101019. https://doi.org/10.1016/j.eclinm.2021.101019
[7] Yendewa, G. A., Perez, J. A., Patil, N., & McComsey, G. A. (2022). HIV Infection is Associated with Higher Risk of Post-Acute Sequelae of SARS-CoV-2 (PASC) However Vaccination is Protective. Social Science Research Network. https://doi.org/10.2139/ssrn.4276609
[8] Peluso, Michael J.a; Antar, Annukka A.R.b. Long COVID in people living with HIV. Current Opinion in HIV and AIDS 18(3):p 126-134, May 2023. | DOI: 10.1097/COH.0000000000000789