By: Marcus J. Hopkins, Founder & Executive Director, Appalachian Learning Initiative
In December 2021, a Ryan White Part B caseworker contacted me to ask whom I knew in the West Virginia Housing Opportunities for Persons With AIDS (HOPWA) state's office. In the few months prior to this request, the Part B office had been beset with clients reaching out to their Ryan White HIV/AIDS Program (Ryan White) caseworkers in frustration and desperation:
"I've been trying to reach my HOPWA caseworker for three months, and nobody will call me back."
"I filled out the paperwork in June, but I haven't heard anything back, and it’s October."
"My electricity was just disconnected after HOPWA didn't pay the bill for three months."
"I've received an eviction notice after HOPWA didn't pay the rent for two months in a row."
"The sober living facility has told me that if HOPWA doesn’t come through with my rent payments, I’ll have to find another place to live."
It turned out that this inability to reach HOPWA caseworkers was not isolated to clients—the Ryan White caseworkers and West Virginia state officials were unable to get responses, either. In the midst of a global pandemic, when having stable housing meant the difference between being able to quarantine and being out in the elements with no protection, one of West Virginia's HOPWA grantees has all but collapsed, leaving clients scrambling to find solutions to problems they were promised would be solved and other state and federal programs scrambling just as desperately to pick up the pieces.
What is HOPWA, and How Does it Work for Grantees and Patients…or Not?
The HOPWA program was created in 1992 through the AIDS Housing Opportunity Act to address the critical housing needs of lower-income Americans living with HIV and their families (AIDS Housing Opportunity Act, 1992). This Act situated the HOPWA program in the U.S. Department of Housing and Urban Development (HUD), making it one of the only HIV-related services and assistance programs situated outside of the U.S. Department of Health and Human Service (HHS). It is also the only program dedicated to the housing needs of People Living with HIV/AIDS (PLWHA).
HOPWA is funded through two mechanisms:
1. Formula Grants:
Ninety percent (90%) of the allocated HOPWA funds are dedicated to what HUD defines as formula grantees, including states and cities within metropolitan statistical areas or jurisdictions, which either administer the funds themselves or sub-contract with local agencies. Health Centers can partner with these local grantees and agencies. THESE GRANTS ARE NON-COMPETITIVE!
2. Competitive Grants:
Ten percent (10%) of the funds fall under competitive grants, which can be awarded to state and local governments and non-profit organizations. Competitive grants are only awarded when funds are available after formula contracted grants are renewed. This means that funds can be administered by a range of entities for each community, from local HIV/AIDS service providers to city and state housing and community development departments or public health departments, and/or partnerships with health centers. (Corporation for Supportive Housing, 2018).
The funds, themselves, are designated for the following purposes:
- The acquisition, rehabilitation, or new construction of housing units
- Costs for facility operations
- Rental assistance and short-term payments to prevent homelessness.
- The coordination and delivery of support services including (but not limited to):
- Assessment and case management
- Substance abuse treatment
- Mental health treatment
- Nutritional services
- Job training and placement assistance
- Assistance with daily living (HUD Exchange, 2022a)
In 2016, outgoing President Barack Obama signed the Housing Opportunity Through Modernization Act (HOTMA) in an effort to better address housing needs across the various HUD-situated housing programs, including HOPWA (HOTMA, 2016). One of the primary changes to HOPWA included revising the statute to include “people living with HIV” rather than just those living with a clinical diagnosis of "AIDS". This effectively changed the formula from:
- Original Formula - # of cumulative AIDS cases
to:
- Modernized Formula - # of people living with HIV/AIDS (and other factors)
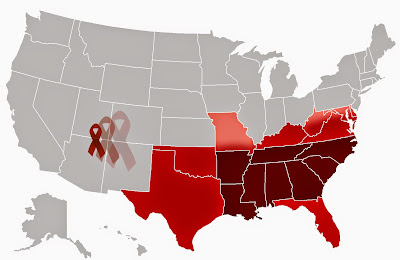
The change to the formula that determines funding essentially means that funds can and will shift according to the geographic jurisdictions with the highest incidence of people living with HIV from year to year. It also set a new baseline for eligible jurisdictions of 2,000 living HIV/AIDS cases. Additionally, it removed the requirement that 25% of funds be distributed to cities based on AIDS incidence and introduced a new requirement that 25% of funds be distributed based on local Fair Market Rents (FMRs) and poverty rates (HUD Exchange, 2017)
Figure 1. HOPWA Formula Modernization Through the Housing Opportunities Through Modernization Act
 |
| Source: HUD Exchange, 2017 |
How HOPWA Works for Grantees But Fails People Living With HIV
From the very outset, it should be made clear that the HOPWA program, along with virtually every resource available on the Internet, is geared not toward PLWHA (read: "clients" or "patients"), but toward Grantees. From the patient's perspective, finding even basic information about the HOPWA program, one’s eligibility for the program, how to apply, whom to contact, or how to resolve issues with grantees is a Sisyphean task. This issue is further complicated by the fact that there are no comprehensive lists of grantees, contact information, service provision, application processes, or housing availability.
Approximately 7% of Ryan White HIV/AIDS Program (RWHAP) clients had temporary housing, and nearly 5% had unstable housing in 2020, with the highest reported housing-insecure age groups being those aged 20-39. Just 72.7% of RWHAP clients experiencing housing insecurity are retained in care. 76.8% of patients experiencing housing insecurity achieved viral suppression in 2020 (Health Resources and Services Administration, 2021). Because of this, stable housing is vital for achieving and maintaining viral suppression in order to decrease the transmission of HIV in the United States.
Most HOPWA grants are non-competitive, meaning that the funds are automatically awarded to specific jurisdictions based on the formula outlined in Figure 1. Those funds are then either administered directly by those jurisdictional governments or regranted and disbursed to contracted organizations within the jurisdiction to provide direct services. The competitive granting process is contingent upon whether or not any funds remain after the non-competitive grants are awarded.
Part of what makes this process frustrating for both patients and grantees is that federal allocations for HOPWA are low relative to the actual cost of housing. For the 2017-2018 Fiscal Year (FY 2017-2018), total HUD funding amounted to $54.66 billion (HUD, 2019b). Of that, $351.5 million—just 0.6% of the total HUD Congressional allocation (Figure 2)—was dedicated to the HOPWA Program (HUD, 2019a).
Figure 2. United States Department of Housing and Urban Development Funding, FY 2018
Sources: HUD, 2019a and 2019b
This low level of federal funding for the only housing program designed explicitly for PLWHA means that grantees are only able to serve a limited number of households (meaning one patient per household). Even if patients are lucky enough to figure out how to apply for the HOPWA program, they are very likely to encounter waiting lists in virtually every jurisdiction. An excellent example of this exists in the state of Delaware:
In 2021, Delaware received a total of $1,951,658 in HOPWA funding (HUD Exchange, 2022b):
- $1,160,648 in Formula grants
- Delaware (Balance of the State) – $336,185
- Wilmington, DE – $824,463
- $791,010 in Competitive grants
- Ministry of Caring (Wilmington, DE)
While Delaware has 3,483 PLWHA living in the state (Delaware Department of Health and Social Services, 2021), its HOPWA program currently serves approximately 150 households—just 4% of the state’s PLWHA population (Delaware HIV Consortium, n.d.). Despite serving just 150 households.
Delaware is one of the more straightforward states to examine. In Ft. Lauderdale, FL, we received reports of 8-year-long waiting lists to fill just a handful of spots. These waiting lists will only grow as PLWHA live longer, earn less, and remain financially eligible for the program.
Attempting to Find Patient-Friendly HOPWA Information
As part of this research effort, the Appalachian Learning Initiative (APPLI, pronounced "apply") conducted a web search to find state-level information about HOPWA programs across the United States and Puerto Rico. Using the search term "[STATE NAME] apply for HOPWA", APPLI searched for state-sponsored websites that provide patient-centered content, including:
- HOPWA Program Information
- Services Provided
- Eligibility Criteria
- Application Processes
- Required Documentation (e.g., identification, income verification, proof of HIV status, et cetera)
- Regional Office Contact Information
- State Office Listing and Contact Information
- Grantee Listing and Contact Information
- Processes for Client-Initiated Complaints
This search was restricted to state-level sites rather than jurisdiction- and grantee-level websites. While 27 states had websites with patient-centered content, just 8 states (FL, GA, IA, ME, NM, OR, SC, and WA) met at least 6 of the 8 information criteria. Twelve (12) states had no state-level HOPWA information (Figure 3 & Appendix 1). Download Appendix 1.
Figure 3. State Housing Opportunities for Persons With AIDS (HOPWA) Websites
Source: Appalachian Learning Initiative
While most states had some HOPWA information available on state-level websites, just 21 state websites listed the names of HOPWA grantees and subgrantees in the state, and only 18 provided contact information for those grantees. Moreover, only 12 state websites provided information about the application process and/or the documents required to apply. Virtually no website mentioned the number of clients served, the status of waitlists or the current wait times on those lists, or outlined a complaint process for client-initiated grievances (e.g., reporting grantees that fail to remit payments in a timely manner). Another unique factor to illustrate was that, for many states, finding these information points required downloading and searching multipage documents filled with complicated processes clearly designed for grantees, rather than patients (APPLI, 2022).
The Need for a Better Resource
The primary issue that APPLI’s research has uncovered is a vast dearth of patient-centered and patient-friendly information available to PLWHA about the HOPWA program. It is, essentially, a program that serves relatively few clients compared to the number of patients in need of housing assistance. This has created an environment where HIV advocates consistently highlight the need for more funding but rarely examine how PLWHA are impacted by how those funds are allocated, disbursed, and utilized.
With this in mind, the Appalachian Learning Initiative has entered into the planning phase of developing a national HOPWA Directory and a patient-centric HOPWA research initiative.
This idea is in its infancy, but I firmly believe that the patient voice is vital to initiating change, as with most public health issues. There will be obstacles to overcome—funding for these initiatives being one of the greatest—but ensuring that patients are easily able to access information about housing assistance for PLWHA is most certainly worth the effort.
Stay tuned for more information as it becomes available.
References:
- AIDS Housing Opportunity Act, 42 U.S.C. Ch. 131 §§12901-12912 (1992). http://uscode.house.gov/view.xhtml?path=/prelim@title42/chapter131&edition=prelim
- Appalachian Learning Initiative. (2022, June 07). State Housing Opportunity for Persons with AIDS Websites. Unpublished.
- Corporation for Supportive Housing. (2018). HUD Policy Brief: Understanding the Impact and Potential for Health Centers. New York, NY: Corporation for Supportive Housing. https://www.csh.org/wp-content/uploads/2018/03/CSH_HUD-Briefs_-HOPWA.pdf
- Delaware Department of Health and Social Services. (2021, January 22). DELAWARE HIV SURVEILLANCE REPORT FOR CASES DIAGNOSED THROUGH DECEMBER 2019. New Castle, DE: Delaware Department of Health and Social Services: Department of Public Health: Health Data and Statistics: HIV Statistics – Epidemiology/Surveillance Profile. https://www.dhss.delaware.gov/dhss/dph/epi/files/2020hivepiprofile.pdf
- Delaware HIV Consortium. (n.d.). HIV Housing Programs. Wilmington, DE: Delaware HIV Consortium: Housing Programs. https://www.delawarehiv.org/housing-programs/
- Department of Housing and Urban Development. (2019a). FY 2020 CONGRESSIONAL JUSTIFICATIONS: COMMUNITY PLANNING AND DEVELOPMENT: HOUSING OPPORTUNITIES FOR PERSONS WITH AIDS (HOPWA). Washington, DC: United States Department of Housing and Urban Development: Program Offices: Chief Financial Officer: Reports. https://www.hud.gov/sites/dfiles/CFO/documents/2020CJ-HOPWA.pdf
- Department of Housing and Urban Development. (2019b). FY 2020 CONGRESSIONAL JUSTIFICATIONS: INTRODUCTION. Washington, DC: United States Department of Housing and Urban Development: Program Offices: Chief Financial Officer: Reports. https://www.hud.gov/sites/dfiles/CFO/documents/2020CJ-INTRODUCTION.pdf
- Health Resources and Services Administration. (2021, December). Ryan White HIV/AIDS Program Annual Client-Level Data Report 2020. Rockville, MD: United States Department of Health and Human Services: Health Resources and Services Administration: HIV/AIDS Bureau: Division of Policy and Data. https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/data/rwhap-annual-client-level-data-report-2020.pdf
- Housing Opportunities Through Modernization Act, Pub. L. No. 114-201, § (a) 130 Stat. 782 (2016). https://uscode.house.gov/view.xhtml?req=%22Housing+Opportunity+Through+Modernization+Act%22&f=treesort&fq=true&num=0&hl=true&edition=prelim&granuleId=USC-prelim-title42-section1437
- HUD Exchange. (2017, July 17). HOPWA Modernization: What Communities Need to Know. Washington, DC: United States Department of Housing and Urban Development: HUD Exchange: Trainings. http://www.meeting-support.com/downloads/244402/10944/PPT%20V2.pdf
- HUD Exchange. (2022a). HOPWA Eligibility Requirements. Washington, DC: United States Department of Housing and Urban Development: HUD Exchange: Programs: Housing Opportunities for Persons With AIDS. https://www.hudexchange.info/programs/hopwa/hopwa-eligibility-requirements/
- HUD Exchange. (2022b). HUD Awards and Allocations: HOPWA. Washington, DC: United States Department of Housing and Urban Development: HUD Exchange: About Grantees: Awards and Allocations. https://www.hudexchange.info/grantees/allocations-awards/?params=%7B%22limit%22%3A20%2C%22COC%22%3Afalse%2C%22sort%22%3A%22%22%2C%22min%22%3A%22%22%2C%22years%22%3A%5B%5D%2C%22dir%22%3A%22%22%2C%22grantees%22%3A%5B%5D%2C%22state%22%3A%22%22%2C%22programs%
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.





.png)
.png)