Guest Blog By: Marcus J. Hopkins, Consultant, Community Access National Network (CANN)
The 2018 midterm election was remarkable in several ways: over 47% of registered voters participated in this election – the highest turnout since 1966 which saw 49% (Domonoske, 2018); the Democratic Party regained control of the House for the first time since 2011; a record number of women won seats in the House (Watkins, 2018); two women became the first Native American women elected to Congress (Watkins); two other women became the first Muslim women elected to Congress (Watkins); Jared Polis became the first openly gay man to be elected governor of a state in Colorado. But something else historic happened, as well – Idaho, Nebraska, and Utah joined Maine in begin the only states to expand Medicaid under the Affordable Care Act (ACA) via a ballot initiative (Pramuk, 2018). And these states are pretty deeply Red.
 |
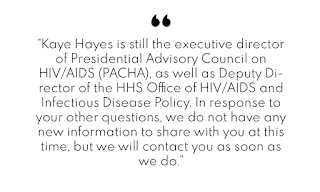
| Photo Source: Political Dig |
For those unfamiliar with Maine’s Medicaid debacle, here is a quick rundown: Maine votes adopted a Medicaid expansion via a ballot initiative in November 2017 which required the submission of a state plan amendment within 90 days and implementation within 180 of the measure’s effective date (which would have been April 03, 2018). Maine’s famously cantankerous and curmudgeonly outgoing Governor Paul LePage (see pictured above) – who vehemently opposed expanding Medicaid – failed to meet that deadline, illegally ignoring the will of the voters – he famously stated he would go to jail before allowing Maine to expand Medicaid (Miller, 2018), and took the issue to court where he has been repeatedly smacked down by judges who insist that he comply with the law and implement the expansion. Governor-Elect Janet Mills – who campaigned on following the law and authorizing the Medicaid expansion and was elected in the 2018 midterm elections – appeared in court on Wednesday, November 07, to listen to arguments in an advocacy group’s case against the Maine Department of Health and Human Services (Bleiberg, 2018).
What is troublesome about the myriad refusals of LePage to abide by the law is that it may have just been a prelude to how Republican governors in these Conservative states may attempt to thwart the will of the voters in Idaho, Nebraska, and Utah. To be fair, two of these governors has in some capacity stated they will abide by the will of the voters: Governor-Elect Brad Little (Idaho) has stated that he will implement the initiative (Guilhem, 2018); Governor Pete Ricketts – just elected for a second term – though a vocal opponent of the measure, has previously stated that if expansion made it onto the ballot, it would be up to the voters (Quinn, 2018). Governor Gary Herbert of Utah vocally opposed Utah Proposition 3, which not only orders the expansion of Medicaid, but implements a prohibition against any changes that would reduce coverage, benefits, or payment rates below policies in place on January 01, 2017.
While these responses are not full-throated endorsements of expansion, they are likely the best we can expect from members of a political party that has vehemently opposed the expansion of Medicaid at almost every turn. The problem with their opposition, however, is that Medicaid expansion – and, in fact, Universal Healthcare in general – are highly popular; even amongst Republican voters, support for Universal/Single-Payer/Medicare-For-All healthcare provided by the government is growing steadily as healthcare costs continue to rise well above the rates of inflation and wage growth.
So, what does Medicaid Expansion mean for the AIDS Drug Assistance Program? Well, a few things:
What we have seen in states that implemented Medicaid Expansion under the ACA is that a significant percentage of ADAP/Ryan White recipients have been shifted off of the Ryan White Program and over to Medicaid. This has had various impacts, both positive and negative, for those who have traditionally relied upon Ryan White and ADAP for payment and coverage of the HIV treatment and medications. Depending upon the way the patient’s state implements Medicaid, they may now be required to pay premiums, deductibles, and/or co-pays for doctor visits and medications that were previously covered by Ryan White and ADAP. That said, Ryan White funds canbe used to cover those costs (HIV/AIDS Bureau, 2014).
Patients living in states that have not expanded Medicaid often have to wait for an AIDS diagnosis in order to qualify for Medicaid coverage, even if they meet the income threshold. Additionally, certain states may also require that patients’ Viral Load or CD4 T-Cell numbers meet a specific threshold, as well, meaning that, if a patient’s Viral Load falls below or CD4 T-Cell count rises above the designated threshold for approval, they may lose their eligibility for coverage. This was my case in West Virginia before the state expanded Medicaid. Expanding Medicaid means that people living with HIV no longer have to wait for an AIDS diagnosis in order to qualify for Medicaid coverage (so long as their income is below the threshold).
The shifting of these patients off of Ryan White ADAP budgets has resulted in lower expenditures on drugs and other HIV treatment costs, which allowed the Ryan White Program to begin providing payment for private health insurance for all Ryan White clients using Ryan White funds through insurance assistance. Only three states do not provide this service – Texas, Idaho, and Mississippi. With the expansion of Medicaid in Idaho, this may allow the program the resources to begin doing so.
In order to shift clients off of Ryan White and onto Medicaid, a client’s income must fall within the specified percentage of the Federal Poverty Level (FPL) respective to each state’s guidelines. In most expansion states, that threshold is 138% of the FPL ($16,753.20 per year for an individual). This percentage for eligibility for Ryan White ranges from 200% (Idaho, Iowa, and Texas) to 550% (South Carolina), which is much more forgiving than the Medicaid requirements.
An additional issue can arise with patients who have been shifted onto Medicaid, as well. While the Ryan White Program was designed solely to focus on the needs of people living with HIV, Medicaid – which is the largest payor for HIV services in the United States – was not designed specifically with the needs of HIV patients in mind. There may be something of a barrier to care and treatment that exists when patients who are used to dealing with Ryan White staff who are familiar with the social, psychological, and medical needs of HIV patients are suddenly expected to communication with Medicaid employees who may not be sensitive to or accommodating of the unique needs of people living with HIV. While it may seem small, that simple communication barrier can lead to lower adherence to medication regimens, missed appointments, and falling out of the continuum of care. The National Alliance of State and Territorial AIDS Directors (NASTAD) holds numerous Technical Assistance conferences and meetings throughout each year where Medicaid directors and staff can attend various workshops and plenary sessions that teach them better ways to approach people living with HIV and to increase cultural competence when dealing with this population.
In general, Medicaid expansion has been a boon for the Ryan White and ADAP Programs. Hopefully, the transition to expanded Medicaid coverage in Idaho, Nebraska, and Utah will be smooth, and people living with HIV will gain access to more options to treat their disease and lead happier, healthier lives.
References:
- Bleiberg, J. (2018, November 07). Day after election, Mills makes her presence felt at court hearing on Medicaid expansion. Bangor, ME: Bangor Daily News: Politics. Retrieved from: https://bangordailynews.com/2018/11/07/politics/day-after-election-mills-makes-her-presence-felt-at-court-hearing-on-medicaid-expansion/
- Domonoske, C. (2018, November 08). A Boatload Of Ballots: Midterm Voter Turnout Hit 50-Year High. Washington, DC: National Public Radio: Elections. Retrieved from: https://www.npr.org/2018/11/08/665197690/a-boatload-of-ballots-midterm-voter-turnout-hit-50-year-high
- Guilhem, M. (2018, September 26). Brad Little, Idaho's GOP Gubernatorial Candidate, Will Support Medicaid Expansion – If It Passes. Boise, ID: Boise State Public Radio. Retrieved from: http://www.boisestatepublicradio.org/post/brad-little-idahos-gop-gubernatorial-candidate-will-support-medicaid-expansion-if-it-passes#stream/0
- HIV/AIDS Bureau. (2014, June 06). Clarifications Regarding Use of Ryan White HIV/AIDS Program Funds for Premium and CostSharing Assistance for Medicaid. Rockville, MD: HIV/AIDS Bureau: Health Resources and Services Administration. Retrieved from: https://hab.hrsa.gov/sites/default/files/hab/Global/pcn1306medicaidpremiumcostsharing.pdf
- Miller, K. (2018, July 12). LePage says he’ll go to jail before he lets Maine expand Medicaid without funding. Portland, ME: The Portland Press Herald. Retrieved from: https://www.pressherald.com/2018/07/12/paul-lepage-says-hed-go-to-jail-before-he-expands-medicaid/
- Pramuk, J. (2018, November 07). Three red states vote to expand Medicaid during an election where health care was the top issue. Englewood Cliffs, NJ: CNBC: Politics. Retrieved from: https://www.cnbc.com/2018/11/07/utah-idaho-and-nebraska-approve-medicaid-expansion-ballot-measures.html?utm_campaign=KHN%3A%20First%20Edition&utm_source=hs_email&utm_medium=email&utm_content=67300319&_hsenc=p2ANqtz-_CWMrFMnVoHCXsdJhMXO7EHWikEaOn0ZFysQJPsMaAA6YjuHvlZp_TKaDDJvAMQg_QQJqAxVB_M3toFbTcXFF0L8RXaQ&_hsmi=67300319
- Quinn, M. (2018, November 07). Red-State Voters Opt for Obamacare. Washington, DC: Governing [dot] com: Topics: Health and Human Services. Retrieved from: http://www.governing.com/topics/health-human-services/gov-medicaid-expansion-voters-ballot-november-states.html
- Watkins, E. (2018, November 07). Women and LGBT candidates make history in 2018 midterms. Atlanta, GA: CNN: Politics. Retrieved from: https://www.cnn.com/2018/11/07/politics/historic-firsts-midterms/index.html
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.