By: Ranier Simons, ADAP Blog Guest Contributor
The ongoing Covid-19 pandemic is a glaring reminder of the importance of the global efforts to address other epidemics and pandemics. After over 30 years of such efforts, worldwide there has been success with polio. Wild poliovirus was virtually extinct in 2020 with only about 140 cases remaining.[1] However, two serious remaining global disease crises are HIV/AIDS and Hepatitis C (HCV).
In 2020, it was estimated that there were 37.7 million people living with HIV/AIDS, and an estimated 58 million people with chronic Hepatitis C.[2][3] The strongest two-pronged approach to fight both is testing and treatment. In 2014, UNAIDS, the Joint United Nations Programme on HIV/AIDS, came up with a target known as 90-90-90. The goal was to have 90% of all persons living with HIV/AIDS aware of their status, 90% of all diagnosed on sustained antiretroviral treatment, and for 90% of those on treatment to have an undetectable viral load by 2020.
The WHO, World Health Organization, proposed a similar target for HCV in 2016. They pledged to globally eliminate HCV by 2030. This elimination included a target of 80% those with HCV to be in treatment, a 90% reduction in new infections, and a 65% reduction in liver-associated deaths as a result of hepatitis C.[4]
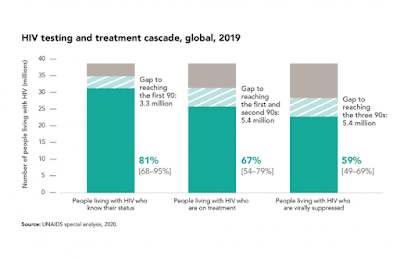 |
| Photo Source: UNAIDS |
The 90-90-90 goal was not met in 2020 and it is not likely that HCV will be eradicated by 2030. Were the goals too ambitious or was there something missing in the execution of the efforts?
The focus has always been on testing and treatment. It is of the utmost importance to have widespread testing to identify those that need treatment in order to get them into treatment. However, what had previously been missing was discourse on barriers to testing and treatment. In 2021, the UNAIDS Global AIDS Strategy acknowledged the existence of structural barriers to HIV and HCV testing and services.
The challenge has been that solving the problem of these hurdles has not been included in the system of testing and treatment. The structural hurdle of lack of fulfilment of basic needs should be a systemic part of treatment. Human nature prioritizes stable shelter, food, and safety over seeking out testing and adherence to treatment regimens.
This is especially true in the population of people who inject drugs (PWID). Intravenous drug users are 29% more at risk to contract HIV and 40% of new HCV infections worldwide.[5]
 |
| Photo Source: Yahoo! |
In response to understanding the importance of including the effective meeting of basic needs as part of disease prevention, a new target, 100-100-100 is being discussed in global health circles. It is initially being considered through the lens of PWID regarding HIV and HCV. The goal is to have stable housing for 100% of PWID who have housing instability, offering substance abuse treatment to 100% of PWID that desire treatment, and giving 100% of PWID access to harm reduction services.
Stable housing means safe and consistent shelter. It means having a stable place to eat and prepare meals. Having stable housing provides a place for self-care and identity. Stress is lowered when one has a safe stable place to live as well allowing focus on other needs. A sense of community results from stable housing as well. When groups of PWID have stable housing, they can create a sense of belonging and care for each other communally.
Having a stable place to live and rest also facilitates successful substance abuse treatment. Taking away stressors of basic survival allows a person to redirect their energies towards bettering their lives. Coupled with substance abuse treatment is harm reduction. Harm reduction services come in many forms.[6] Most importantly it is acknowledging the complicated etiology of drug use. It is the realization that drug use does happen, and it is necessary to help people along the continuum of complete abstinence from drug use to the other end of safer and “responsible” drug use starting at whichever stage PWID find themselves.
Reaching this 100-100-100 goal, along with aggressive strides toward testing and treatment, is the growing discourse that is providing hope towards the eradication of HIV and HCV. Removing the inequalities of lack of basic needs will help not just PWID but the greater population at large living with HIV and HCV as well.
[1] Kaiser Family Foundation. (2021, Oct 29). The U.S. Government and global polio efforts. Retrieved from https://www.kff.org/global-health-policy/fact-sheet/the-u-s-government-and-global-polio-efforts/
[2] UNIADS. Global HIV and AIDS statistics fact sheet. Retrieved from https://www.unaids.org/en/resources/fact-sheet
[3] World Health Organization. (2021, Jul 27). Hepatitis C. Retrieved from https://www.who.int/news-room/fact-sheets/detail/hepatitis-c
[4] World Health Organization. (2016). Global health sector strategy on viral hepatitis 2016-2021. Towards ending viral hepatitis. World Health Organization. Retrieved from https://apps.who.int/iris/handle/10665/246177
[5] UNAIDS. (2017, Jan 1) 90–90–90: an ambitious treatment target to help end the AIDs epidemic. Retrieved from https://www.unaids.org/en/resources/documents/2017/90-90-90
[6] Principles of harm reduction. National Harm Reduction Coalition. Retrieved from https://harmreduction.org/about-us/principles-of-harm-reduction/
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.






