By: Brandon M. Macsata, CEO, ADAP Advocacy Association
The ADAP Advocacy Association hosted an HIV/AIDS "Fireside Chat" retreat in Wilmington, North Carolina among key stakeholder groups to discuss pertinent issues facing people living with HIV/AIDS. It was the first Fireside Chat in over two and a half years, after they were suspended in response to the ongoing Covid-19 pandemic. The Fireside Chat took place on Thursday, June 16th, and Friday, June 17th. Utilization Management, Ending the HIV/AIDS Epidemic (in the South), and Covid-19's Impact on Public Health were evaluated and discussed by 22 diverse leaders in the fight against the HIV/AIDS epidemic.
 |
| Photo Source: Getty Images |
The Fireside Chat included moderated white-board style discussion sessions on the following issues:
- Utilization Management: What is its Impact on Patient Access to Care and Treatment — moderated by Murray Penner, U.S. Executive Director, Prevention Access Campaign (PAC)
- Ending the Epidemic (EHE): What is its Impact in the South — moderated by Lee Storrow, National Policy Director, Community Education Group (CEG) & Board Chair, Southern AIDS Coalition (SAC)
- Covid-19: What is its Impact on HIV, Viral Hepatitis, Sexually Transmitted Infections (STIs), and Substance Use Disorder — moderated by Jen Laws, President & CEO, Community Access National Network (CANN) & Board Member, ADAP Advocacy Association
The discussion sessions were designed to capture key observations, suggestions, and thoughts about how best to address the challenges being discussed at the Fireside Chat. The following represents the attendees:
- Guy Anthony, Founder, Black, Gifted & Whole
- De' Shea Coney, HepConnect Coordinator, North Carolina AIDS Action Network
- Tori Cooper, Director of Community Engagement, Human Rights Campaign
- Dawn Patillo Exum, Director of Public Policy, Merck
- Jasmine Ford, HIV Clinical Coordinator, Virginia Department of Health
- Dusty Garner, Board Member, Community Access National Network
- Aquarius D. Gilmer, Associate Director, Corporate Policy & Alliances, Gilead Sciences
- Marcus J. Hopkins, Founder & Executive Director, Appalachian Learning Initiative
- Tim Horn, Director, Health Care Access, National Alliance of State & Territorial AIDS Directors (NASTAD)
- Venton Jones, Chief Executive Officer, Southern Black Policy & Advocacy Network
- Jen Laws, President & CEO, Community Access National Network
- Brandon M. Macsata, CEO, ADAP Advocacy Association
- Judith Montenegro, Program Director, Latino Commission on AIDS
- Murray Penner, Executive Director, North America, Prevention Access Campaign
- Kalvin Pugh, Sr. Manager, Community Engagement at International Association of Providers of AIDS Care
- Alan Richardson, Executive Vice President of Strategic Patient Solutions, Patient Advocate Foundation
- Carl Schmid, Executive Director at HIV + Hepatitis Policy Institute
- Robert Skinner, Advocate — Florida
- Cindy Snyder, Director, Government Relations, ViiV Healthcare
- Lee Storrow, National Policy Director, Community Education Group
- LaWanda Wilkersaon, Advocate — North Carolina
- Joey Wynn, Chairman, Florida HIV/AIDS Advocacy Network (FHAAN)
The Covid-19 pandemic is still ongoing, and accordingly to The New York Times (as of June 14th), “The average number of new cases in the United States fell to 98,867 yesterday, a 2 percent decrease from the day before. Since January 2020, at least 1 in 4 people who live in the United States have been infected, and at least 1 in 330 people have died” (NYT, 2022).
With that in mind, the ADAP Advocacy Association implemented strong Covid-19 safety protocols for the Fireside Chat, which included proof of vaccination/booster, robust self-administered testing (prior to travel, upon arrival, and after returning home), complimentary rapid self-test kits and hand sanitizer for each of the attendees, as well as guidelines for masks on commercial travel to the event, and optional masks during the sessions (which some attendees exercised without feeling shunned).
At the meeting's outset, a signature fishing vest with its AIDS red ribbon owned by the late Bill Arnold, longtime President & CEO of the Community Access National Network (CANN), was gently placed on one of the chairs in the room. It was meant to symbolize that Bill would always have a seat at the table in an honorary way to pay tribute to the decades of advocacy work done on behalf of people living with HIV/AIDS dating back to the 1980s. There wasn't a dry eye in the room!
 |
| Bill Arnold, August 13, 1938 - September 29, 2021 |
The ADAP Advocacy Association is pleased to share the following brief recap of the Fireside Chat.
Utilization Management (UM):
According to Penner: "UM is a process that payers and healthcare plans utilize to evaluate the medical necessity, appropriateness, and efficiency of the use of health care services (medicines, procedures, etc.). There are valid reasons for UM (particularly medical necessity), but UM is also often used to help contain costs and to deny coverage of high cost meds and procedures in favor of lower cost alternatives. With HIV medications, in particular, it often restricts access to medications that providers and patients have determined as necessary for appropriate care and treatment. UM practices in theory are appropriate for safety and continuity of care, but far too often they have become discriminatory and present challenges to accessing medications and remaining adherent to them."
Penner's discussion on UM started with a broad overview of the practice, including examples, clinical efficacy, and provider feedback. It also included the impacts of UM on patient access, Ending the Epidemic efforts, and viral suppression, as well as the statutory and regulatory protections and limitations.
Prior authorization is probably the most commonly-known technique exercised by payers, but many others exist. An important part of the conversation centered around a recent survey on prior authorization released by the American Medical Association (AMA), 2021 AMA prior authorization (PA) physician survey.
The survey found, sadly, that one in four patients often abandon their recommended course of treatment, and a staggering "82% report that PA can at least sometimes lead to treatment abandonment." The survey focused on patient impact, but it also featured relevant information on physician impact and employer impact. The survey results can be found online at https://www.ama-assn.org/system/files/prior-authorization-survey.pdf.
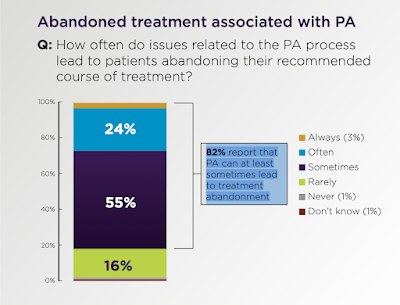 |
| Photo Source: American Medical Association |
Patients needing to complete eligibly "recertification" under the State AIDS Drug Assistance Program (ADAP) was also a hot topic of conversation. Most States require the bureaucratic red tape be rolled-out every six months, which is widely accepted as unnecessary. Fortunately, some flexibility was recently authorized by the Health Resources & Services Administration (HRSA) on the ADAP recertification process. The Virginia Department of Health, for example, is extending their program recertification to every 24 months!!!
Other UM-related issues discussed included drug formularies, convoluted Rx refill cycles, safety protections afforded to patients (i.e., drug contraindications), and the "prescriber prevails" provisions under New York Medicaid.
The following materials (partial list) were shared with retreat attendees:
- American Medical Association - 2021 AMA prior authorization (PA) physician survey. American Medical Association
- American Medical Association - Prior Authorization and Utilization
- Centers for Medicare and Medicaid - CCIIO Regulations and Guidance
- Harvard Health Publishing - Do generic drugs compromise on quality?
- Health Affairs - Quantifying The Economic Burden Of Drug Utilization Management On Payers, Manufacturers, Physicians, And Patients
- Journal of Managed Care & Specialty Pharmacy - The Effect of Formulary Restrictions on Patient and Payer Outcomes: A Systematic Literature Review
- AIDS and Behavior - The Demand for Antiretroviral Drugs in the Illicit Marketplace: Implications for HIV Disease Management Among Vulnerable Populations
- NBC News - Transgender people report years of battles for health insurance coverage
The ADAP Advocacy Association would like to publicly acknowledge and thank Murray for facilitating this important discussion.
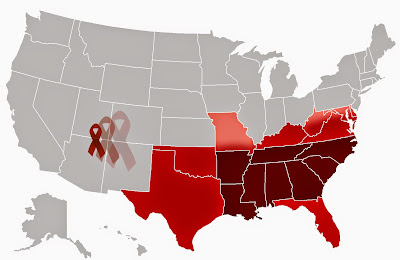
Ending the HIV Epidemic (in the South):
The Ending the HIV Epidemic (EHE) in the United States initiative has been front and center among HIV advocacy circles since it was announced during a previous president's State of the Union. According to the U.S. Centers for Disease Control & Prevention (CDC), "The EHE initiative is scaling up four science-based strategies that can end the epidemic: Diagnose, Treat, Prevent, and Respond. For maximum impact, CDC is continuing to invest in communities most affected by HIV — to help local HIV programs recover, rebuild, and begin to expand EHE strategies in the wake of COVID-19."
Lee Storrow summarized it more clearly as, "Refocusing limited resources to target the hot spots." Despite the EHE initiative being characterized by some advocates as off to a middling start, it does still represent the first new influx of significant federal dollars in quite some time. Of particular importance to this discussion was EHE's footprint in the South (and Appalachia), which is disproportionately impacted by HIV/AIDS.
Of course, one of the biggest - and still ongoing - topics of intense conversation center around why some apparent hot spots are included under the EHE initiative, while others were excluded. For example, West Virginia. Neither West Virginia nor any of its 55 counties were included as Phase 1 jurisdictions of the EHE initiative. Considering the state has two enduring, intertwined epidemics, West Virginia's exclusion highlighted some of the initiative's shortcomings.
According to Storrow: "The participants of the fireside chat had a wealth of big ideas about how we could make a big impact when it comes to HIV rates in the South and Appalachia. Ending the Epidemic isn’t just a reference to the plan and funding source, it’s a mindset to catalyze new energy and bring new resources to bare to combat HIV. When I was working in HIV advocacy in North Carolina, we took advantage of the moment in time the announcement of the federal EHE created to get new state funding from the NC General Assembly. We’ve got to leave it all on the line and leave no stone unturned to make sure the HIV advocacy community has the resources and tools to get this work done."
Storrow's discussion on EHE (in the South) included a history of the initiative, as well as where we are today fighting the epidemic in the South and in Appalachia. Discussions centered around targets (and whether they'll be met), disruptions caused by Covid-19, state-level EHE plans, and future federal EHE expansion to include other jurisdictions.
 |
| Photo Source: ADAP Advocacy Association |
Storrow also used the session to raise awareness about the Opioid Settlement Plans that are currently unfolding nationwide. It led to a lively conversation about how those settlement dollars could be leveraged to boost public health programs that specifically impact HIV, viral hepatitis, sexually-transmitted infections, and substance use disorder programs.
Other EHE-related issues discussed included social determinants of health, and ongoing challenges to achieve better health equity.
- The Hill - Pandemic disrupted HIV prevention efforts, CDC report says
- NPR - Lessons From HIV On Ending The COVID Pandemic
- Office of the Honorable Shelley Moore Capito - CAPITO URGES HHS SECRETARY TO INCLUDE WEST VIRGINIA IN INITIATIVE TACKLING HIV EPIDEMIC; WV initially excluded from federal program aimed at helping communities most affected by HIV
- North Carolina Health News - Mecklenburg among top focus locations in Trump HIV plan
- North Carolina Health News - Zero new HIV cases: the goal for Mecklenburg County
- North Carolina Department of Health and Human Services - NCDHHS Urges Testing During National HIV Testing Day, Releases End the HIV Epidemic Plan
- North Carolina Department of Health and Human Services - NC ENDING THE EPIDEMIC: A Plan to End HIV Together Community-by-Community Hand-in-Hand
- Opioid Settlement Tracker - STATES' OPIOID SETTLEMENT ALLOCATION PLANS
Covid-19's Impact on Public Health:
In early 2021, Jen Laws penned a blog evaluating the mess being caused by the Covid-19 pandemic. At that time, Laws argued, "Covid-19 has also clearly highlighted the impact of social determinants of health and health disparities of which HIV and HCV [Hepatitis C] advocates have long been aware." He was right, and unfortunately not much as changed 18 months later.
According to Laws: "Public health has taken on new, both exciting and unfortunate, shapes as a result of our collective responses to Covid-19. The expanded use of telemedicine has helped modernize our access to care while also leaving those in more rural areas and impoverished communities of the country at distinct disadvantage due to lack of infrastructure, threatening to widen already existing health disparities. Defining a still shifting landscape as Covid-19 related flexibilities and legal changes, presents numerous challenges to public health as an industry and public health professionals will be digesting these changes and challenges for years, if not decades, to come. This is as true, if not more true, for pre-Covid-19 public health programs focused on infectious disease, including STIs, HIV, and viral hepatitis, as these infrastructures and personnel continue to face uncertain futures in politically hostile environments."
Laws' discussion on Covid-19 impact included background context on the state of public health programs pre-Covid-19, as well as related changes to public health and public health programs. It included discussion on the current and future state of the public health programs important to the HIV community. Some of the key questions asked included: What changes do we want to keep? What changes do we need to do away with? How do we evaluate the paradigm shift in publics' mood toward public health (i.e., anti-science, anti-vaccination)?
 |
| Photo Source: CDC |
The stated goal of the session was "to define the impacts of COVID-19 on public health infrastructure and programs." It celebrated flexibility and innovation offered by various temporary governmental regulation and the “forced modernization” of health care in many situations – namely, telehealth. Of dire concern, however, are these flexibilities are threatened to end as the public health emergency winds down, including the continuous coverage requirement for Medicaid programs under the public health emergency declaration. Some attendees also stressed that there are downsides to relying on telehealth, especially for rural communities lacking the necessary infrastructure to make health care accessible.
CDC's own HIV surveillance data proves earlier Covid-19 concerns, which was regularly noted.
- Community Access National Network - Community Roundtable Emphasizes Impacts of COVID-19 (2021)
- Community Access National Network - Community Roundtable Defines the Shape of Public Health Advocacy Amid COVID-19 (2022)
- Centers for Disease Control and Prevention - Impact of COVID-19 on STDs. Sexually Transmitted Disease Surveillance 2020
- National Association of County and City Health Officials - NACCHO Requests Protection of Public Health department Officials and Staff from Harassment, Intimidation, and Threats of Violence
- NBC News - Because of Covid, 2020 was a ‘lost year’ in the fight against HIV, report suggests
- Kaiser Health News - Strides Against HIV/AIDS Falter, especially in the South as Nation Battles COVID
- Kaiser Family Foundation - Delivering HIV Care and Prevention in the COVID Era: A National Survey of Ryan White Providers
The ADAP Advocacy Association would like to publicly acknowledge and thank Jen for facilitating this important discussion.
Additional Fireside Chats are planned in September 2022 (Chicago, Illinois).

No comments:
Post a Comment