By: Ranier Simons, ADAP Blog Guest Contributor
Population health decisions should always be evidence-based and informed by quality data. State AIDS Drug Assistance Programs (ADAPs), funded by the Ryan White HIV/AIDS Program (RWHAP), provide access to HIV antiretrovirals and other related prescription medications to low-income people living with HIV/AIDS (PLWHA) who are uninsured or underinsured. They also offer other support services that bolster PLWHA’s ability to manage HIV care. Without regard to its inherent value, the Trump Administration's FY2026 budget proposal calls for cuts to the RWHAP, which could adversely affect patients served by ADAPs. A recent study of longitudinal data proves that ADAPs are efficacious and valuable, deserving of more funding, not less (McManus, 2025).
 |
| Photo Source: MedRxIV |
A recent study, led by Dr. Kathleen McManus of the University of Virginia School of Medicine, evaluates how ADAPs have contributed to the United States' viral suppression rates from 2015 to 2022. The findings show that ADAPs are effective and their viral suppression outcomes are better than those of PLWHA, who do not receive ADAP-funded services.
The retrospective longitudinal study explored ADAP participants’ viral suppression (VS) and viral load (VL) data compared to the PLWHA overall population from 2015 to 2022. The state-level data covered all 50 states and the District of Columbia, sourced from the National Alliance of State and Territorial AIDS Directors (NASTAD) National RWHAP Part B and ADAP Monitoring Project Annual Reports and the Centers of Disease Control and Prevention’s (CDC) National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) AtlasPlus (McManus, 2025). All jurisdictions for each year of the study were considered, only including data for a jurisdiction when the NASTAD and CDC data for any given year were both complete. Establishing set guidelines for data inclusion strengthened the validity of the findings.
 |
| Photo Source: NASTAD |
Over the study period, there were some years where various jurisdictions were not included due to missing data. Overall, 81.9% to 96.4% of the population of PLWHA were included. From 2015 to 2022, the estimated number of PLWHA in the U.S. grew from 942,988 to 1,092,023. The number of ADAP clients from the overall population for each year ranged from 146,879 to 220,839, or 65.5% to 96.9%, respectively (McManus, 2025).
The VS rate for PLWHA overall ranged from 60% to 66.3%. However, the VS rate for non-ADAP participants ranged from 53.2% to 59.4% compared to 81.2% to 91.4% for ADAP clients. This indicates that viral suppression was significantly higher among those served by state ADAPs. This finding is significant given that for the entire study period, ADAP clients were underrepresented among those eligible for assessment (McManus, 2025). In other words, the proportion of PLWHA ADAP clients overall was always higher than the proportion eligible for VS assessment. Additionally, for all the study years, the proportion of PLWHA who were ADAP clients was greater than the proportion of PLWHA who were ADAP clients with detectable VL. Notably, in 2020 and 2022, the proportion of ADAP clients was only 5.7%, although ADAP clients comprised 23.9% and 21.0%, respectively, for both years (McManus, 2025).
Consistently, ADAP clients comprised one-third (~33%) of all virally suppressed PLWHA nationwide while representing only 21.0% to 24.4% of the total PLWHA population (McManus, 2025). This data illuminates that ADAPs result in higher VS rates than the VS rates of the general population of PLWHA. The cost of HIV antiretroviral medications is not decreasing (McCann et. al, 2020). Moreover, PLWHAs live longer; thus, there is an increasing demand for assistance from ADAPs (McManus et al., 2013). It is not in the best interest of public health nor fiscal responsibility to cut funding to ADAP programs.
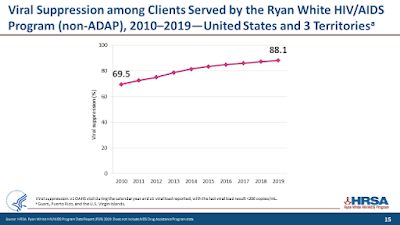 |
| Photo Source: HRSA |
It would be wiser to increase funding and establish policies that expand and innovate using RWHAP and ADAP funds. Viral suppression increases with ADAP-supported health insurance (McManus et. al, 2019). Supporting expanded ADAP enrollment efforts in addition to ADAP-covered premiums would expand access compared to the costs of providing medication directly for those without any insurance. Cutting RWHAP funds and subsequently ADAP funding would result in the loss of medication and care access for many PLWHA. Disruptions in medication and care access would decrease VS rates and potentially increase transmission rates and poor health outcomes. One CDC study showed that 63% of new HIV transmissions resulted from 34% of PLWHA who were aware of their status but were not virally suppressed (Li et. al, 2016).
Achieving viral suppression is the most effective way to prevent HIV transmission. “Undetectable = Untransmittable” (U=U) is one of the most essential tenets of HIV treatment and prevention. U=U is possible because of the lifesaving and life-changing medications that ADAPs can provide. Federal funding for ADAPs has remained flat for years, especially for southern states (Nunn, 2014). Cutting funding would be detrimental to state ADAPs across the board. The study, headed by Dr. McManus, should be a data-rich wake-up call for policymakers aiming to reduce funding.
[1] Li, Z., Purcell, D., Sansom, S., Hayes, D., Hall, H. (2016). Vital Signs: HIV Transmission Along the Continuum of Care - United States. MMWR Morb Mortal Wkly Rep. 2019;68(11):267-272. doi:10.15585/mmwr.mm6811e1.
[2] McCann, N., Horn, T., Hyle, E., Walensky, R. (2020, February 3).HIV Antiretroviral Therapy Costs in the United States, 2012-2018. JAMA Intern Med. 2020;180(4):601–603. doi:10.1001/jamainternmed.2019.7108. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2759735#:~:text=School%2C%20Boston%2C%20Massachusetts-,JAMA%20Intern%20Med.,3
[3] McManus, K., Christensen, B., Nagraj, V., Furl, R., Yerkes, L., Swindells, S., Weissman, S., Rhodes, A., Targonski, P., Rogawski McQuade, E., & Dillingham, R. (2019). Evidence From a Multistate Cohort: Enrollment in Affordable Care Act Qualified Health Plans’ Association With Viral Suppression. Clinical Infectious Diseases, 71(10), 2572–2580. https://doi.org/10.1093/cid/ciz1123. Retrieved from https://academic.oup.com/cid/article/71/10/2572/5627781
[4] McManus, K., Engelhard, C., & Dillingham, R. (2013). Current challenges to the United States' AIDS drug assistance program and possible implications of the Affordable Care Act. AIDS research and treatment, 2013, 350169. https://doi.org/10.1155/2013/350169. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3614023/#:~:text=The%20demand%20for%20ADAP%20support,goals%3B%20and%20the%20recession%20continues.
[5] McManus, K., Killelea, A., Rogers, E., Liu, F., Horn, T., Steen, A., Keim-Malpass, J., Hamp, A., & Rogawski McQuade, E. (2025). State AIDS Drug Assistance Programs’ Contribution to the United States’ Viral Suppression, 2015-2022. https://doi.org/10.1101/2025.04.04.25325288. Retrieved from https://www.medrxiv.org/content/10.1101/2025.04.04.25325288v1.full.pdf
[6] Nunn, A. (2014, May). The Southern Epidemic: Are the South’s cultural, political and societal barriers making it difficult for public health programs, such as the AIDS Drug Assistance Programs, to function effectively in this region? Retrieved from https://www.adapadvocacy.org/pdf-docs/2014_aaa_WP_The_Southern_Epidemic_05-15-14.pdf
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.

No comments:
Post a Comment