By: Ranier Simons, ADAP Blog Guest Contributor
Medical debt continues to be a crippling financial burden to many Americans, with most of the debt being owed to hospitals in the United States. Approximately 100 million adults have medical debt ranging from $500 to over $5,000.[1] Despite changes credit reporting agencies made in 2022, 15 million Americans still have more than $49 billion in unpaid medical collections on their credit reports.[2] Medical debt is a financial hindrance to many aspects of people’s lives and can even result in poor healthcare outcomes and denial of care. The evolution of medical debt relief efforts continues to move forward on the federal and state levels in hopes of unsaddling Americans of debt that they had no choice in incurring.
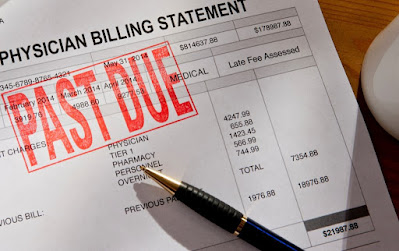 |
| Photo Source: Rhode Island Currant | Getty Images |
In response to a 2022 report conducted by the Consumer Financial Protection Bureau (CFPB), three nationwide credit reporting bureaus - Equifax, Experian, and TransUnion – voluntarily made changes to reduce the number of reported medical bills in collections. They increased the time span that trigger reporting of medical bills in collections from 180 days to one year, stopped reporting and removed bills less than $500, and stopped reporting bills that were previously bad debt in collections but had been paid, thus resolved.[2] Despite these actions, 15 million Americans are still plagued with unpaid medical collections on their credit reporting.
In an attempt to further help Americans, CFPB proposed new rules in June 2024 that would be significant if finalized. The rules would eliminate the special medical debt exception, establish guardrails for credit reporting companies, and ban repossession of medical devices.[3] The CFPBs intent is “to end the senseless practice of weaponizing the credit reporting system to coerce patients into paying medical bills that they do not owe.”[3] These rules would help close existing loopholes that leave medical debt accessible to creditors. Additionally, since much of the collection activity reported is inaccurate, it would prevent predatory collections on false claims. Most of the people who have medical collections on their reports do not have any history of other types of credit problems.[4] It is unfair for creditors to block people from the things that they need when the CFPB found that a medical bill on a credit file is not a good indicator of the likelihood a person will repay a loan.[3]
The Urban Institute has done a great deal of work aggregating medical debt data. They created an interactive mapping tool, which shows the geography of debt in America and the debt differences that can reinforce the wealth gap between white communities and communities of color. Nationwide, roughly five percent of Americans have unpaid medical debt based on their credit reports.[5] However, the South and people of color carry a disproportionate amount of that debt. For example, in North Carolina, 8.5% of the population has medical debt in collections compared to 5% nationally. In terms of demographic distinction, 10.5% of communities of color in North Carolina have bad medical debt in contrast to 7.8% of white communities.[5]
 |
| Photo Source: Carolina Journal |
Following the trajectory of other states, the administration of Governor Roy Cooper in North Carolina created a plan to alleviate medical debt in the state. With the federal government's support, Governor Cooper created the model for a plan that would link Medicaid expansion dollars to patient debt. Medicaid expansion provides billions in funding for hospitals through state-directed payments that states use to pay hospitals to care for low-income patients.[6] Governor Cooper created a plan that penalizes hospitals, reducing the Medicaid expansion funds they would receive if they do not agree to his debt-relief plan.
Hospitals would have to expand financial aid criteria to allow more patients to qualify for aid to stave off a future of debt, in addition to eliminating old debts of low-income patients.[6] Eliminating debt would occur via debt buy-back in the manner non-profits such as Undue Medical Debt have succeeded.[6] In essence, bad debt is purchased at extreme discounts and then written off. By agreeing to the plan, hospitals would gain almost twice as much funding as they would if they did not. Atrium Health would receive roughly $1.7 billion by participating, compared to $900 million if they did not.[6] Atrium Health has been historically very aggressive with debt collection efforts against patients. In agreement with Cooper’s plan, Atrium Health announced it would nullify all existing judgments and liens against patients for unpaid bills, some going back as far as twenty years.[7]
Numerous reports have showcased how some large hospital systems have practiced aggressive collection and billing activity against vulnerable low-income patients in conflict with their fiduciary requirements to exercise charity care and institute patient financial assistance. Most of the medical debt is specifically hospital debt.[8] According to a report published by the Robert Wood Johnson Foundation, nearly 75% of adults with medical debt owe some or all of it to hospitals.
 |
| Photo Source: Urban Institute | RWJF |
Brenda Miller with the Lown Institute previously argued in a blog, "Hospitals have the choice to offer robust financial assistance, set reasonable prices, not sue patients, and pay their fair share in community benefits if they are nonprofit. By adjusting their policies, hospitals have the power to alleviate the long-term financial suffering caused by our broken healthcare system."[9]
As a part of the continuing examination of the burden of medical debt, this week, ADAP Advocacy launched an online survey to collect data on patient perspectives and experiences with medical debt. It is available nationwide for anyone in the United States to participate. It is also anonymous with the option of providing personal information if you wish to be contacted for additional follow-up.
The ADAP Advocacy-sponsored Ryan White Grantee 340B Patient Advisory Committee commissioned the study to support patient-centered reform. Many hospitals, as recipients of drug rebates under the 340B Drug Pricing Program, are notoriously bad actors. Data from the survey will add color to patients’ lived experiences with medical debt’s whole-person effect on their lives.
Many types of consumer spending are voluntary. Most medical spending is not. When one’s health and well-being are threatened, potential financial ruin should not add stress to decisions nor influence them. Capitalism-driven financial toxicity has no place in healthcare. Hospitals should be institutions of optimal healing for all. As Jen Laws (he/him/his), CEO of Community Access National Network, points out, “...equity-minded persons and entities prioritizing impact over intent is a very real thing.”[10]
Read our related blog, Are Nonprofit Hospitals' Community Benefit Tax Breaks Truly Serving Communities in Need?
[1] Vankar, P. (2024, January 31). Medical debt in the U.S. - Statistics & Facts. Retrieved from https://www.statista.com/topics/8219/medical-debt-in-the-us/#topicOverview
[2] Consumer Financial Protection Bureau. (2024, April 29). CFPB Finds 15 Million Americans Have Medical Bills on Their Credit Reports. Retrieved from https://www.consumerfinance.gov/about-us/newsroom/cfpb-finds-15-million-americans-have-medical-bills-on-their-credit-reports/
[3] Consumer Financial Protection Bureau. (2024, June 11). CFPB Proposes to Ban Medical Bills from Credit Reports. Retrieved from https://www.consumerfinance.gov/about-us/newsroom/cfpb-proposes-to-ban-medical-bills-from-credit-reports/
[4] Pollitz, K. (2015, Jan 8). Medical Debt Among Insured Consumers: The Role of Cost Sharing, Transparency, and Consumer Assistance. Retrieved from https://www.kff.org/health-costs/perspective/medical-debt-among-insured-consumers-the-role-of-cost-sharing-transparency-and-consumer-assistance/
[5] Urban Institute. (2024, July 10). The Changing Medical Debt Landscape in the United States. Retrieved from https://apps.urban.org/features/medical-debt-over-time/
[6] Levey, N., Alexander, A. (2024, September 23). How North Carolina Made Its Hospitals Do Something About Medical Debt. Retrieved from https://kffhealthnews.org/news/article/north-carolina-hospitals-medical-debt/?utm_campaign=KHN%3A%20First%20Edition&utm_medium=email&_hsenc=p2ANqtz-9_BieSj5YKhMJyyO8tuHpBuD1MMqvTUIH1qbLMpxBqXd2wLyVlWUhNZuMd1TjH99Epf8GJEgAie1fXAtiopyrJGRkkQg&_hsmi=325818163&utm_content=325818163&utm_source=hs_email
[7] Crouch, M., Ledger, C. (2024, September 20). Atrium Health cancels thousands of past medical debt judgments
[8] Karpman, Michal. (March 2023). MOST ADULTS W ITH PAST-DUE ME DICAL DE BT OWE MONEY TO HOSP ITAL. Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/insights/our-research/2023/03/most-adults-with-past-due-medical-debt-owe-money-to-hospitals.html
[9] Miller, Brenda. (2023, March 28). Are Hospitals Driving Medical Debt? The Lown Institute. Retrieved from https://lowninstitute.org/are-hospitals-driving-medical-debt/
[10] Laws, J. (2023, June 19). The Necessity of Patient-Centered 340B Reform. Retrieved from https://www.hiv-hcv-watch.com/blog/june-19-23
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.

No comments:
Post a Comment