By: Ranier Simons, ADAP Blog Guest Contributor
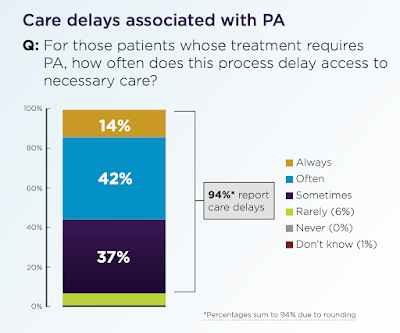
Amidst all the complicated machinations of the U.S. healthcare system, the ultimate focus should be the patient's best interests. Unfortunately, many barriers interfere with physicians and patients working together for the most optimal outcomes. One of those pervasive barriers is prior authorization. Prior authorization (PA) is when insurers require healthcare providers to obtain pre-approval for things such as services, procedures, durable medical goods, and medications. The pre-approval is required before insurance companies will agree to pay for a requested intervention. Insurance industry messaging claims that prior approvals are in the best interests of patients to make sure that inappropriate care is not needlessly utilized, thus saving them money, lowering healthcare system expenditures, and ensuring only the most effective options for care are chosen by physicians.
 |
| Photo Source: Salon (Getty Images/FG Trade) |
However, PAs are not in patients' best interests but are a method of cost control or cost-cutting to save insurers money. Jen Laws, CEO of Community Access National Network, states, “Taking a note from auto carriers, payers have been utilizing prior authorization as a bet that most folks don't have time, energy, or navigation experience enough to fight for the care patients rightly need. It's delay and deny on the bet that patients will give up." PAs have detrimental effects on patient health outcomes, interfere with the patient-physician relationship, unduly burden physicians, and ultimately generate more healthcare spending, because of medical interventions needed because of the poor patient outcomes they can cause.
For several years, many groups have been fighting for prior authorization reform. Recently, in a step in the right direction, the Centers for Medicare and Medicaid Services (CMS) released their Final Prior Authorization and Interoperability Rule (CMS-0057-F).[9] Even though it is a win for patients and providers, it is not enough. As such, legislatures nationwide are working on state-level legislative remedies to the prior authorization problem. Some states have already passed more stringent measures, and others have bills in process.[6]
The new rule has many details, but there are some notable highlights. A significant problem with the prior authorization process is the excessive time burden placed on medical providers.[1] According to a 2022 American Medical Association (AMA) survey, physicians and their staff spend an average of about 14 hours, roughly two business days per week, completing around 45 PAs per physician.[7] Historically, much of the PA process is manual, requiring long phone calls and forms to be filled out, faxed, or sent through postal mail. The CMS rule helps with this by requiring insurers to support an electronic prior authorization process that is embedded in the physician’s electronic health records. This streamlines the process and helps with automation since the electronic health record is a centralized place where physicians do much of their work. Patients regularly see their physician typing things like notes and prescription requests in the examination room during their visits.
 |
| Photo Source: American Medical Association |
Another remedy the new CMS rule delivers is transparency. When PAs are often denied, physicians and patients don’t know why since the insurers don’t give clear reasoning. They respond with opaque responses such as deeming a requested medical intervention as ‘medically unnecessary’. The new rule requires insurers to give very specific reasons for denial. This will not only enable providers to refute and appeal denials more effectively but can result in more accountability of insurers. Having to provide precise reasoning will result in insurers being more cautious with denials. CMS furthers transparency requirements by requiring metrics reporting. The new rule requires insurers to publicly report their actions such as how often they approve and deny PAs, how long they take to make decisions, as well as the frequency of denials and approvals by medical ailment category. This will enable patients to be informed consumers as they shop for insurance coverage.
The new CMS rule has many positive details but also limitations. The ruling does not pertain to prescription drugs. The ruling also only applies to government-regulated health plans such as Medicaid, CHIP, Medicaid managed care plans, and plans on the healthcare exchange. The electronic PA requirement goes into effect in 2027, and the metric reporting goes into effect in 2026. To create more substantial changes, some states have already passed PA reform legislation, and many others are working on it. The District of Columbia has already passed legislation with some of the same aspects as the CMS ruling, but also goes further.
The District of Columbia passed Bill 25-124, which became ACT 25-301 in November 2023.[5] The act has an electronic PA requirement in the same manner as the CMS rule. It requires all review entities to accept and respond to PA requests using their NCPDP SCRIPT Standard ePA transaction by January 1, 2024.[5] The D.C. Act goes beyond the CMS ruling regarding required timeframes for PA decisions. The CMS ruling requires review entities to respond within 72 hours for expedited urgent care PA requests and within seven days for standard requests. The D.C. Act requires review entities to respond within 24 hours with approval or denial of urgent care PA requests.[5] For standard requests, it specifies a response within three business days by electronic portal or five business days by mail, fax, or telephone.[5]
North Carolina is one of the states with pending PA legislation. Its details also contain some requirements that are more stringent than those of CMS. Like the D.C. Act, one highlight is its timetable for review response specification. For non-urgent healthcare services PA requests, an insurer must decide within 48 hours of obtaining all required information and within 24 hours for urgent care requests.[10] The North Carolina bill also contains transparency language. Suppose the reviewing entity of an insurer questions the medical necessity of a physician’s PA request. In that case, it must notify the provider within five business days of the date of the request.[10] Also, before issuing a PA denial, the insurer must allow the affected provider to discuss the need for the medical service on the telephone directly with the medical doctor who will be responsible for the review determination.[10]
 |
| Photo Source: American Medical Association |
Current and developing state legislation model suggestions supported by the AMA. One of those is “gold carding”. Five states have already passed gold carding legislation: Louisiana, Michigan, Texas, Vermont, and West Virginia.[6] In gold carding, six months of a medical practice or provider’s prior authorizations are reviewed. If 90% of the requests are approved, then that practice or provider is not subject to any PA requirements for six months.[6,8] Maintaining those statistics would be required to maintain the privilege. While on the surface, it seems to be a good way to reduce the volume of PAs, thus reducing administrative time waste, it has a downside. As Jen Laws points out, “Gold carding can come with the incentive for payors to become even more aggressive in their PA and other UM (utilization management) practices because it rests on the idea that a provider can "prove" they don't need review. The best way around that is to merely get more aggressive with UM, moving the goalpost to an unattainable standard.”
The adverse effects of prior authorizations are well documented. They cause physician burnout, interfere with the patient-provider relationship, and cause delays in patient care.[3,7] Delays in patient care can result in avoidable poor patient health outcomes and exacerbation of disease states.[2,3,4] In diseases such as cancer, timely and very personalized treatment can be a matter of life and death. Physicians make very informed decisions about their patients’ medical care. When physicians make evidence-based treatment determinations for their patient's best health, they should not be undermined by profit-centric cost-cutting measures that are not based on proper consideration of current medical data. Pushing forward to ensure transparency and accountability is critical. It will take continued federal and state efforts to create a healthcare landscape that genuinely has the patient at its center.
[1] Medical Ecconomics. (2023, August 4). 2023 Physician Report: The latest physician salary, productivity and malpractice cost data. Retrieved from https://www.medicaleconomics.com/view/2023-physician-report-the-latest-physician-salary-productivity-and-malpractice-cost-data?slide=18
[2] Sausser, L. (2023, December 2023). Cancer patients face frightening delays in treatment approvals. Retrieved from https://kffhealthnews.org/news/article/cancer-patients-prior-authorization-treatment-delays/
[3] Merrill, J. R., Flitcroft, M. A., Miller, T., Beichner, B., Clarke, C. N., Maduekwe, U. N., Wang, T. S., Dream, S., Christians, K. K., Gamblin, T. C., Evans, D. B., & Kothari, A. N. (2023). Patterns of Unnecessary Insurer Prior Authorization Denials in a Complex Surgical Oncology Practice. The Journal of surgical research, 288, 269–274. https://doi.org/10.1016/j.jss.2023.03.013
[4] Miller, T. (2023, November 7). Big insurance met its match when it turned down a top trial lawyer's request for cancer treatment. Retrieved from https://www.propublica.org/article/blue-cross-proton-therapy-cancer-lawyer-denial#:~:text=Blue%20Cross%20and%20Blue%20Shield%20denied%20payment%20for%20the%20proton,he%20was%20ready%20to%20fight.
[5] Council of the District of Columbia. (2023, November 15). D.C. ACT 25-301 Prior Authorization Reform Amendment Act. Retrieved from https://lims.dccouncil.gov/downloads/LIMS/52301/Signed_Act/B25-0124-Signed_Act.pdf?Id=180462
[6] Sable-Smith, B. (2024, February 12). States target health insurers' 'prior authorization' red tape. Retrieved from https://kffhealthnews.org/news/article/states-health-insurers-prior-authorization-legislation-gold-carding/
[7] American Medical Association. (2023). 2022 AMA prior authorization (PA) physician survey. Retrieved from https://www.ama-assn.org/system/files/prior-authorization-survey.pdf
[8] American Medical Association. (2024, January 24). Advocacy in action: Fixing prior authorization. Retrieved from https://www.ama-assn.org/practice-management/prior-authorization/advocacy-action-fixing-prior-authorization
[9] Centers for Medicare and Medicaid Services. (2024, January 17). CMS Finalizes rule to expand access to health information and improve the prior authorization process. Retrieved from https://www.cms.gov/newsroom/press-releases/cms-finalizes-rule-expand-access-health-information-and-improve-prior-authorization-process
[10] North Carolina General Assembly. House Bill 649 - Ensure Timely/Clinically Sound Utiliz. Review. Retrieved from https://www.ncleg.gov/Sessions/2023/Bills/House/PDF/H649v0.pdf
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.

No comments:
Post a Comment