By: Ranier Simons, ADAP Blog Guest Contributor
HIV criminalization laws represent the worst of society’s response to the AIDS epidemic, rooted in fear, homophobia, and hysteria…and a lot of misinformation. The United States was the first nation to enact HIV-specific criminal laws, dating back to 1986-87. HIV criminalization laws still exist, but the wheels of progress are slowly chipping away at them as medical advances have changed HIV/AIDS from a death sentence to a manageable chronic disease. Equally important is the growing acceptance of the science behind “Undetectable Equals Untransmittable” (U=U), which has weakened the argument for these outdated, inhuman laws. Recently, two states, Maryland and North Dakota, passed bills to remove HIV criminalization laws from their statutes.
 |
| Photo Source: CHLP | The Marshall Project |
Yet, many states still have active HIV criminalization laws in place. From 2008 to 2013, at least 180 people living with HIV/AIDS (PLWHA) were arrested or charged under HIV criminalization laws (Tang, 2024). These HIV statutes have not been updated to reflect evidence-based science and are predatory towards PLWHA. As of February 2025, 32 states have offenses that criminalize exposure to and/or transmission of HIV (CHLP, 2025). In 1994, Texas was the first state to repeal its HIV criminalization law (CHLP, 2020). The reality is that much work remains to kick HIV criminalization laws back to the 1980s, and some states are doing it!
In February of this year, Senate Bill 356 and House Bill 39 passed in both Maryland chambers. Both bills are repeals of a section of the Maryland code that specifically criminalized the intentional transfer of HIV from one person to another. The statute declared the knowing transmission of or attempted transmission of HIV a misdemeanor subject to a fine of up to $2,500 or a jail term with a maximum of three years, or both. Legislators passed the bills with the understanding that the law was not an effective means of protecting public health. Delegate Kris Fair stated (seen below), “The law was, for right or wrong, thought to help curb the transmission of HIV…What public health experts and criminal justice organizations have taught us … is that we’ve actually seen the exact opposite.” (Brown, 2025).
 |
| Photo Source: Maryland Matters | Photo by Danielle J. Brown |
Also, on February 20, 2025, North Dakota passed House Bill 1217. This repeals a section of the code regarding the willful transfer of bodily fluid containing HIV. ‘Transfer’ here is defined as “engage in sexual activity by genital-genital contact, oral-genital contact, or anal-genital contact, or to permit the reuse of a hypodermic syringe, needle, or similar device without sterilization.” The law being repealed states that a person who knowingly transfers HIV to another person without their knowledge can be charged with a Class A felony with a maximum penalty of 20 years in prison and a maximum fine of $20,000. The bill changes the crime from a felony to a misdemeanor (Gall, 2025). In North Dakota, HIV is the only disease attributed to a felony charge, whereas other STI transmission crimes are misdemeanors. The bill now needs to be considered in the House.
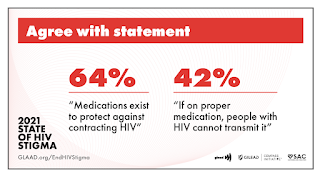
Both states acknowledge that HIV criminalization is discriminatory. Singularly carving out HIV as a disease requiring enhanced criminal penalties increases stigma, is a disincentive for the public to normalize testing, and disproportionately affects specific populations. Fear of potential criminal prosecution means that people will be more hesitant to seek testing and subsequently must disclose their status to their partners (Yang, 2018). Additionally, it can adversely affect the trust within the doctor-patient relationship, resulting in delayed antiretroviral treatment initiation, poorer treatment outcomes, and adversely affecting public health.
Medical science has made the possibility of HIV transmission effectively non-existent by PLWHA, who are undetectable on treatment. “U=U” is not a catchy slogan – it is an evidence-based scientific reality. Requiring an individual to indisputably prove their disclosure of their status if accused of exposure without consent is virtually impossible (Lazzarini, 2013). When HIV criminalization laws are in place, people can nefariously use them against people, such as a spurned partner retaliating against a former partner when a relationship does not end on good terms. Predatory laws harm PLWHA because being convicted does not even require actual HIV transmission to occur or proof of intent to deliberately pass the virus on to someone.
 |
| Photo Source: Red Bubble |
HIV criminalization laws also disproportionately affect marginalized groups, such as communities of color, specifically black men. Racial inequities and social determinants of health have already been shown to increase the likelihood of black male exposure to the criminal legal system (AIDS Vu, 2021). When HIV criminalization laws add enhanced sentencing or create violations that otherwise would not exist, they exacerbate targeted adverse outcomes. In Maryland, for example, Black people are 30% of the population, 71% of those who are PLWHA, and 82% of HIV-related criminal cases. Black men, specifically, are 68% of those accused in HIV-related cases despite comprising only 14% of the state population and 44% of Maryland PLWHA (UCLA, 2024).
Maryland and North Dakota’s recent bills to eliminate HIV criminalization are positive steps, but much more needs to be done. The number of states that currently have laws specifically targeting HIV for violations outside of standard communicable disease statutes or heightened sentencing is unacceptable. The stigma and hindrance to widespread testing of HIV criminalization add to the numerous barriers to ending the HIV epidemic in the United States. It would be easily conquerable if laws would catch up to science.
[1] AIDSVu. (2021, May 10). HIV Criminalization. Retrieved from https://aidsvu.org/news-updates/hivcriminalization/#:~:text=HIV%20criminalization%20laws%20have%20also,transgender%20women%2C%20and%20sex%20workers.
[2] Brown, J. (2025, February 22). Bills to repeal ‘antiquated’ law criminalizing transfer of HIV sail through House, Senate. Retrieved from https://marylandmatters.org/2025/02/22/bills-to-repeal-antiquated-law-criminalizing-transfer-of-hiv-sail-through-house-senate
[3] The Center for HIV Law and Policy (CHLP). (2020). HIV CRIMINAL LAW REFORM: BEFORE & AFTER: Texas. Retrieved from https://www.hivlawandpolicy.org/sites/default/files/HIV%20Criminal%20Law%20Reform%20Before%20and%20After%20Texas%2C%20CHLP%202020.pdf
[4] The Center for HIV Law and Policy (CHLP). (February, 2025). Mapping HIV Criminalization Laws in the U.S. Retrieved from https://www.hivlawandpolicy.org/sites/default/files/2025-02/Mapping%20HIV%20Criminalization%20Laws%20in%20the%20US%2C%20CHLP%202025.pdf
[5] Gall, P. (2025, February 20). House Bill to reduce HIV transmission penalty advances in North Dakota. Retrieved from https://www.ksjbam.com/2025/02/20/intentional-hiv-transmission-charge-may-be-lowered-from-felony-to-misdemeanor/#:~:text=House%20Bill%201217%20passed%20on,to%20the%20Senate%20for%20consideration.
[6] Lazzarini, Z., Galletly, C. L., Mykhalovskiy, E., Harsono, D., O'Keefe, E., Singer, M., & Levine, R. J. (2013). Criminalization of HIV transmission and exposure: research and policy agenda. American Journal of Public Health, 103(8), 1350–1353. https://doi.org/10.2105/AJPH.2013.301267
[7] UCLA School of Law Williams Institute. (2024, January). Enforcement of HIV Criminalization in Maryland. Retrieved from https://williamsinstitute.law.ucla.edu/wp-content/uploads/HIV-Criminalization-MD-Jan-2024.pdf
[8] Tang, Catherine (2024). Our country's dark history of persecuting people with HIV. HIV Plus Magazine. Retrieved from https://www.hivplusmag.com/stigma/us-history-hiv-criminalization.
[9] Yang, Y. T., & Underhill, K. (2018). Rethinking Criminalization of HIV Exposure — Lessons from California’s New Legislation. New England Journal of Medicine, 378(13), 1174–1175. https://doi.org/10.1056/nejmp1716981
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.