By: Ranier Simons, ADAP Blog Guest Contributor
The doctor-patient relationship is the cornerstone of healthcare. Patients cannot fully benefit from the many advances in medical science without a solid relationship with their provider, where they feel listened to and cared for. The relationship has been defined as “a consensual relationship in which the patient knowingly seeks the physician’s assistance and in which the physician knowingly accepts the person as a patient” (Chipedza et al., 2015). Mutual trust and vulnerability are required, especially regarding people who are living with HIV/AIDS (PLWHA). ViiV Healthcare recently released data from the third wave of its Positive Perspectives Research study (PP3), which examines the lived experiences of PLWHA globally. This wave of inquiry is heavily focused on improving health outcomes by digging into the interactions between PLWHA and their healthcare providers.
 |
| Photo Source: GoodTherapy |
The current wave, PP3, will eventually include 3,000 participants. The newly released data is a result of the first 698 participants representing 16 countries, including the United States, United Kingdom, and Canada (Lutton, 2025). Eventually, it will cover 29 countries. Wave One surveyed 1,111 PLWHA and 250 of their partners, covering nine countries. Wave 2 involved 2,389 PLWHA covering 25 countries (ViiV, Press Release 2025). All the waves investigate various themes surrounding the lived experiences of PLWHA. PP3 aims to further define and raise the voices of PLWHA to improve healthcare outcomes by informing healthcare providers and other stakeholders of the realities of how PLWHA navigate their care and day-to-day lives.
Early PP3 data suggest an overarching theme of communication issues between PLWHA and their healthcare providers. The early findings indicate that there are strong levels of trust in PLWHA’s patient-provider relationships. Approximately 80% of those currently surveyed reported trusting their healthcare provider. (Lutton, 2025). However, while the trust is solid, there are reported weaknesses in areas such as patients' practical understanding of information and their inclusion in care decisions.
 |
| Photo Source: Doctor Patient Relationship |
Although a high level of trust has been reported, 47.5% of PLWHA surveyed feel that their healthcare providers do not effectively listen to them, and 39.7% reported that they were not included in the choice of their antiretroviral regimen (ART) (ViiV, 2025). Successful HIV health outcomes are holistic, involving more than just a focus on viral suppression. Patients need to be able to fully express their values, preferences, and individual life circumstances to their healthcare providers. Empathy is associated with patient satisfaction and treatment adherence (James, 2023). When healthcare professionals truly listen, they can better understand how their patients interact with life, which is often vastly different from their own lives and familiar ways of thinking.
Part of ART selection is based on patients’ specific virological needs. However, there are nuances of selection that are influenced by patient preference when patients are fully informed of all their options. The preliminary study results indicated that 53% of patients were worried about long-term effects of ART (ViiV Press Release, 2025). ART comes in many different combinations of drugs with the potential for short-term and long-term side effects. Approximately 53% of respondents had ART-related weight gain as a side effect concern. It is essential for healthcare professionals to engage in transparent discussions about the aspects of different drug combinations, empowering patients to make informed decisions rather than leaving them to accept the physical manifestations of regimens that are unilaterally imposed upon them. Patients’ ability to be consistent with their regimen is also a consideration in education about all modalities, such as long-acting injectables. Approximately 43.2% of the current respondent group stated a disdain for daily medication because it was a daily reminder of their HIV status (ViiV Press Release, 2025). When patients feel fully included in their care, they are more likely to adhere to their medication schedule.
 |
| Photo Source: Patient Voices |
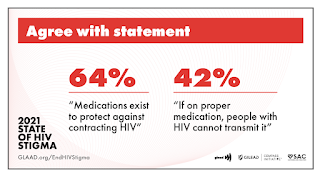
A notable early revelation of the study is that the concept of undetectable equals untransmittable, or “U=U”, is not fully embraced or understood. Medical science has proven that PLWHA cannot transmit the HIV virus when they have reached and maintained an undetectable viral load. However, only 58% of respondents truly believed it. Approximately 93.7% knew U=U, but low uptake of it as a belief system means that many PLWHA are not empowered to fully live their lives without the guilt and stigma of embracing their relationships and sexual expression. Moreover, only 31.1% of patients were able to explain the concept of U=U to other people (ViiV Press Release, 2025). It is essential for healthcare providers to thoroughly educate PLWHA on the science behind U=U, enabling them to advocate for themselves and combat stigma within their social networks.
Wave three of the Patient Perspectives study is only partially complete. The goal of 3,000 participants will yield a more comprehensive picture of the patient-doctor relationship, providing healthcare professionals with an informed understanding of its strengths and weaknesses. Understanding what is being done well in comparison to areas needing improvement will enable providers to make effective changes to the status quo. Health literacy is influenced by socioeconomic status, age, racial and ethnic factors, and educational levels (Dawson-Rose et al., 2016). Once fully completed, PP3 will inform healthcare providers on how to facilitate improvements in patients’ health literacy, as well as bolster care professionals’ ability to step outside their own spheres of understanding into an empathetic place of true patient communication.
[1] Chipidza, F. E., Wallwork, R. S., & Stern, T. A. (2015). Impact of the Doctor-Patient Relationship. The primary care companion for CNS disorders, 17(5), 10.4088/PCC.15f01840. https://doi.org/10.4088/PCC.15f01840
[2] Dawson-Rose, C., Cuca, Y. P., Webel, A. R., Solís Báez, S. S., Holzemer, W. L., Rivero-Méndez, M., Eller, L. S., Reid, P., Johnson, M. O., Kemppainen, J., Reyes, D., Nokes, K., Nicholas, P. K., Matshediso, E., Mogobe, K. D., Sabone, M. B., Ntsayagae, E. I., Shaibu, S., Corless, I. B., … Lindgren, T. (2016). Building Trust and relationships between patients and providers: An essential complement to health literacy in HIV care. Journal of the Association of Nurses in AIDS Care, 27(5), 574–584. https://doi.org/10.1016/j.jana.2016.03.001
[3] James, T. (2023, January 12). Building Empathy into the Stucture of Health Care. Retrieved from https://postgraduateeducation.hms.harvard.edu/trends-medicine/building-empathy-structure-health-care#:~:text=Studies%20demonstrate%20how%20empathy%20improves,they%20feel%20heard%20and%20understood.
[4] ViiV Healthcare. (May 2025). Positive Perspectives Research. Retrieved from https://viivhealthcare.com/hiv-community-engagement/positive-perspectives-research/#:~:text=Wave%203%20survey
[5] ViiV Press Release. (2025, May 27). ViiV Healthcare Positive Perspectives 3 Study Finds Widespread Communication Barriers: Half of People Living with HIV Feel Unheard by Healthcare Providers Despite High Trust. Retrieved from https://viivhealthcare.com/hiv-news-and-media/news/press-releases/2025/may/positive-perspectives-survey/
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.