Life is a circle. I remember spiking high fevers and having strange rashes in the Summer of 1980 while working on a Psychology master’s degree at Stony Brook University. It was a mystery. Cell phones and the Internet did not exist as we know them today. Information was scarce, and LGBQT persons led a shadowy existence. It seemed that attempted suicides were on the rise, and I believed part of the problem was isolation and a general distrust of established counseling centers.
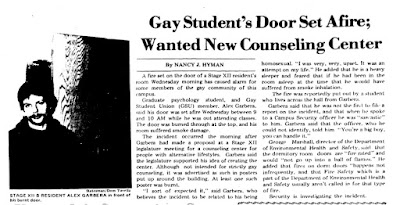
I thought creating a dorm-based counseling service might help individuals struggling with gender and issues of sexuality more accessible. A poster hanging outside my dorm door announcing the first meeting was set on fire. It burned through, and if I had been sleeping at that time, I would probably not be writing this blog today.
 |
| Photo Source: Stony Brook Satesman Vol. 23 No. 61 3/14/1980 |
I was traumatized. The words of the security guard are imprinted in my brain: “You’re a big boy, you can handle it.” It wasn't until the past few years I’ve really become keenly aware of trauma and how it affects us. The counseling project was put on hold and full attention was given to completing my studies, graduation and corporate ladder climbing.
Having always been health conscious, I regularly checked into a STD clinic every six months. Something seemed strange though around 1984. The Long Island free clinic was re-designed and once open cubicles were now fully shielded by plexiglass. Even-though I never tested positive for any STDs, I was told: “you should go to New York City where homosexuals go. I should go to a homosexual clinic.” I hadn’t the slightest clue why or where to go.
Employment brought me to CT instead. I found a gay physician and buried myself in my work. When at a Boston training seminar, I met someone. He wanted to move to CT, and so we decided to begin a healthy relationship, starting off with the new HIV test that just came out in 1986. I tested positive and was shocked, after all, I never had tested positive for any STDs… my partner at the time was extremely supportive. He said it did ‘t make a difference to him as he was putting together a portable BBQ grill. His test results came a week later, also positive. Thus, a journey began but the healthy relationship soon turned out to be anything but. He never wanted to talk about it and didn’t want anyone to know. He acted out by drinking and I acted out by trying to control his drinking. It was a volatile drama that catapulted me into Al-anon to return the focus onto me and my own sanity.
At that time New Haven had a very large, strong, vibrant Gay AA and Gay Al-Anon groups that would periodically have joint meetings and annual convention called a Round-Up. It was a godsend. People talked about everything, well almost everything. Nobody mentioned the words HIV or AIDS, and I knew I wasn’t the only one. There is an Al-Anon slogan “Let it Begin With Me” and so I did start talking about my HIV. First at local group meetings, then at Round-Ups in Connecticut and Provincetown, giving workshops on being HIV positive and in recovery. Over the years individuals would bring it up claiming it saved their life. I was appreciative but always reminded them the life they saved was of their own doing. (I have issues with compliments)
I didn’t do it to help others so much as it was necessary to talk about the feelings of living with HIV, being ejected from a dentist after disclosing my status, navigating life. The gay physician I was seeing frowned when I mentioned taking vitamins and things to boost natural immunity, so I switched to the new HIV clinic at YALE New Haven Hospital.
It was so new they initially did not have a physical space for people with HIV/AIDS. We were combined within the Gerontology clinic. So, there I was a young gay man in his early 30’s, with an oxygen tank breathing aerosolized pentamadine next to an elderly man hooked up to his oxygen tank looking at me very puzzled wondering what I was doing there.
It also seemed that I never got to see the same provider more than once and felt very disconnected from my own care. When I attended a talk by Dr. Gary Blick, MD who mentioned a more holistic, cutting edge and educational approach I knew that as the right match for me.
Life is a circle. Thinking of that old man looking at me seems ironic. I am now a senior, over 65 – but not requiring assisted breathing yet.
In the recent past there have been a slew of workshops/ seminars on HIV and aging, responding to the fact that most people living with HIV are living longer and are now over 50 years old.
This may seem intuitive as medication’s become less toxic and easier to take. It is not as simple as one might assume. A relatively recent study created headlines that “HIV May Speed Up the Body’s Aging Process”
Yet, I am not seeing much structural adaptation to our aging HIV population, and non-HIV related medical research tends to exclude people with HIV.
Accelerated aging issues and increased susceptibility to conditions more prevalent for older persons is not news for those long-term HIV survivors actively engaged in managing their health outcomes. Just as issues of HIV stigma and social isolation echo what many elderly faces.
The accelerated aging process is what horrified people in the early days of the pandemic — before HIV’s discovery — as young gay man was exhibiting symptoms and dying of rare diseases more typical in elderly populations, particularly around the Mediterranean region. Now that we understand more about HIV and people with HIV are living longer there seems to be much less sense of horror giving way to apathy and ageism.
We didn’t have the luxury of apathy “back in the day”— a phrase I lifted from a young nurse asking me questions about the 1980’s before he was born. Death was in our face. People are still dying, but in far fewer numbers. We have also become more clinical about death, even secretive under the cloak of HIPPA and it no longer sparks any outrage.
Back then, radical right preachers said AIDS was sent from God to punish homosexuals and drug users (which probably is still around however unspoken). My response was that if it was sent by God, it was sent as a spotlight on our will to live and love ourselves and each other. Perhaps a test of our compassion and readiness of our social and medical institutions.
 |
| Picture: 2006 |
In a chapter title “Living with Insanity” from Stories From the Other Side: Thematic Memoirs I wrote: “I think HIV/AIDS is here to teach us a few lessons. My fear is that unless we learn them, it is not going to go away and something worse will come along if we keep our heads buried in the sand.” This came from a metaphysical principle that the lesson never goes away until it is learned.
As a spotlight, HIV has and continues to shine light to many of our phobias and isms: homophobia, transphobia, sexphobia, racism, classism, colonialism, ageism (to name a few) and all the intersections where they inevitably meet.
If HIV is viewed as a spotlight on aging, it needs a very wide lens. Covid-19 raised the social isolation alarm to a deafening silence. It wasn’t too long ago that the surgeon warned that loneliness is as dangerous to one’s health and longevity as smoking a pack of cigarettes a day.
Upon hearing this and knowing the issues of increased susceptibility to certain illnesses and cancers correlated with HIV, the U.S. Surgeon General’s report almost made me want to smoke cigarettes.
Of the many diverse long-term survivors, I know one of the shared themes is a strong unmet need for socialization, meaningful social interaction, intimacy, and lighthearted fun.
It is curious that in the early days of HIV there was less funding yet more community activities — at least in CT — such as weekend spiritual retreats, support groups, interfaith services, and healing circles.
While it takes planning and resources to create relevant accessible senior support/socialization groups and creating supportive HIV senior housing, perhaps going back to the early days of HIV buddy programs would be a good/easy place to start?
Another difficult need is finding gerontological expertise in concert with expert HIV care.
These structural changes require educating our aging HIV population as well as using trauma informed care to address complex post traumatic stressors (CPTSD) from accumulated of years of living with HIV. There are many levels of trauma and HIV stigma, and some can be very scarring, making isolation, however deadly, deceptively preferable.
Very early on, when many PLWHAs were given only a few months to live, it was clear that survival alone was insufficient. Quality of life matters.
The word “heal” means “to make whole.” We know what works, and in addition to medication supportive services such as housing, mental health, nutrition is crucial, just as addressing the disparities in health care and outcomes.
There was a time when HRSA funded complimentary therapies such as medical massage, nutritional supplements, chiropractic care and acupuncture. These therapies helped PLWHAs deal with systemic inflammation, medication side effects, pain, and mobility issues.
With the war launched against opiate abuse I see very little of these alternatives coming back — and pain management an increasing nightmare. I wonder why the proceeds from opiate related lawsuits aren’t being channeled back into holistic therapies.
Quality of life also requires integrating life extension research factoring aging issues as well as the metabolic and inflammatory demands HIV incurs. Current programs directed at the health and well-being of clients such as nutritional programs need adjustments accordingly.
HIV Aging issues are not academic. They may seem daunting, but the good news is there is much room for growth, change and novel approaches.
Looking back at everything I would say that one should never underestimate the importance of being able to make a difference in one’s own life and others. Just as Margaret Mead said: “Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it's the only thing that ever has.”
If people were terrified when young persons were getting old people’s diseases and now those young-ins are old, can we re-ignite, or even approach, the same level of urgency, action, and care?