By: Ranier Simons, ADAP Blog Guest Contributor
Long-acting injectable (LAI) agents remain at the forefront of medical innovation, especially regarding HIV treatment and prevention. LAIs are significant because they increase access options for people living with HIV/AIDS (PLWHA) for treatment, opening pathways for sustained viral suppression. LAIs are a solution for PLWHA who experience challenges adhering to daily oral antiretrovirals. Taking pills daily is unduly mentally burdensome as a reminder of living with HIV/AIDS; some patients cannot take daily pills due to stigma and living in an unsafe environment, and many deal with housing instability or travel frequently (New Vision, 2025). Updated study results and other recent developments solidify the efficacy and promise of LAIs as the future of treatment and prevention.
 |
| Photo Source: EATG |
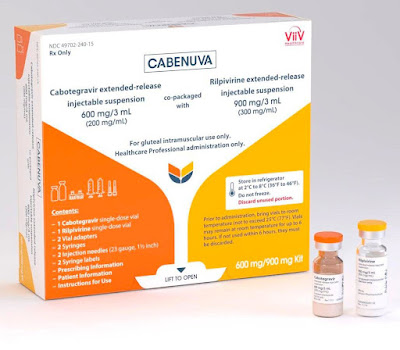
Cabenuva (cabotegravir plus rilpivirine), approved in January 2021, is the first and only complete long-acting injectable and two-drug regimen available for HIV treatment. Initially, it was approved for monthly injection, then expanded to bi-monthly dosing (Haelle, 2025). However, Cabenuva was developed for PLWHA who have already achieved viral suppression before starting use. Ongoing research has been investigating the efficacy of Cabenuva for PLWHA with detectable viral loads, known as viremia.
A recent study led by Ricky Hsu, MD, of NYU Langone Medical Center in New York City, indicates Cabenuva would also be effective for widespread use for PLWHA with viremia (Haelle, 2025). The study group consisted of patients selected from the Observational Pharmaco-Epidemiology Research & Analysis (OPERA) cohort. OPERA includes over 150,000 PLWHA. Among the eligible subjects who were U.S. residents, eighty-eight percent achieved viral suppression. PLWHA with viremia on oral medication need options to facilitate reaching viral suppression, and the study shows the promise of future widespread indications for LAIs to achieve that goal (Haelle, 2025).
Moreover, the final results of the CARES study on LAI antiretroviral therapy in Africa, released in March of this year at the Conference on Retroviruses and Opportunistic Infections (CROI) in San Francisco, further support the efficacy of LAIs. The results were so promising that the World Health Organization (WHO) updated its guidelines to inform that virally suppressed PLWHA on oral medications may switch to Cabenuva because it is equivalent (New Vision, 2025). As future studies confirm the widespread use for PLWHA with viremia, the goal would be for the WHO to add this to its guidelines.
 |
| Photo Source: European Pharmaceutical Review |
While very effective, Cabenuva must be administered in a medical office setting, as it is given through intramuscular injection. The requirement of travel to a clinic setting is a potential barrier for PLWHA, particularly those with transportation challenges, especially if they do not live near a conveniently located facility. A study led by Eric Meissner, M.D., Ph.D., at the Medical University of South Carolina (MUSC) examined the possibility of LAI injections in a home setting (MUSC, 2025). The project gave thirty-three participants the option to receive injections in a clinic setting or at home. Eighteen chose the home setting.
In the home setting, eighteen PLWHA were visited by licensed practical nurses (LPNs) who gave the injections. Meissner’s group arranged for pharmacies to mail LAIs to patients, along with instructions to store the medication in their refrigerators until LPN arrival. Patients were highly satisfied, indicating that home administration is a plausible way to enhance patient adherence. Home injections would be more challenging on a widespread level, given the logistics necessary to coordinate pharmacy with staffing LPNs to visit homes (MUSC, 2025). Moreover, insurance does not reimburse for the staff coordination of pharmacy and nurse visits. Making home LAI administration commonplace would require innovation of funding infrastructure as well as staffing solutions.
 |
| Photo Source: Tu Salud |
Cabenuva is a beneficial first step in the widespread use of LAIs for HIV treatment; however, it is not universally appropriate. Some PLWHA cannot use Cabenuva because they have resistance to non-nucleoside reverse transcriptase inhibitors (NNRTIs). The rilpivirine component of Cabenuva is an NRRTI (Haelle, 2025). One possible solution is the use of lenacapavir (Sunlenca) in addition to Cabenuva. Sunlenca is a semi-annual LAI used for people on oral antiretroviral treatment who have multiple-drug resistance issues. However, the future of long-acting agents should also include other options, such as those that are oral. One option under study is a weekly dosage of an oral combination of islatravir, a nucleoside reverse transcriptase translocation inhibitor, and lenacapavir (Haelle, 2024).
Eliminating HIV has required and will continue to require multiple tools of treatment. Current utilization of LAIs will lead to the development of new injectables and non-injectable long-acting agents. The variety of available therapies needs to keep up with the increasing variance in the characteristics of PLWHA in need of treatment. Continued research and funding innovation will be necessary to ensure the rapid growth of LAIs, and other non-injectable long-acting agents continues.
[1] Haelle, T. (2024, March 11). Once-Weekly ART Showed Similar Efficacy for HIV as Daily ART. Retrieved from https://www.medpagetoday.com/meetingcoverage/croi/109111
[2] Haelle, T. (2025, August 4). The Future of ART Regimens for HIV Is in Long-Acting Agents. Retrieved from https://www.msn.com/en-us/health/other/the-future-of-art-regimens-for-hiv-is-in-long-acting-agents/ar-AA1JTX8S?ocid=socialshare
[3] New Vision. (2025, August 6). Long-acting injectable HIV treatment as effective as daily oral pill — study. Retrieved from https://www.msn.com/en-xl/news/other/long-acting-injectable-hiv-treatment-as-effective-as-daily-oral-pill-study/ar-AA1K4slS?ocid=socialshare
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.
.png)
.png)
.png)






.png)