By: Ranier Simons, ADAP Blog Guest Contributor
Lenacapavir, a novel HIV treatment medication, again appears in the medical news cycle. A recent article in Medical Express, ‘FDA approves treatment for multi-drug resistant HIV,’ was published on September 1st.[1] The article title would lead the reader to think the drug was just approved. However, the U.S Food and Drug Administration (FDA) initially approved lenacapavir in December of 2022.[2] Gilead Sciences released the medication under the name Sunlenca. Please view the previous ADAP Advocacy discussion of Sunlenca and its background here. So, what happened?
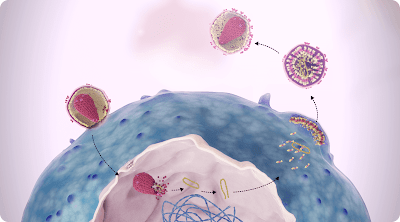 |
| Photo Source: sunlencahcp.com |
The impetus for the recent article is newly reported data regarding lenacapavir’s ongoing clinical trials. The August 2023 issue of The Lancet included the story, 'HIV presents an article where researchers discuss week 52 results of the phase 2/3 trial',[3] which discusses the study's results. But just as important is examining the study’s design.
The ongoing clinical trial of lenacapavir is also known as the Capella study, ClinicalTrials.gov number NCT04150068. There are 72 subjects divided into two cohorts. Previous data had been reported for evaluations performed at 26 weeks. In Cohort 1, 36 subjects were randomly assigned oral lenacapavir or placebo on days 1,2, and 8 in addition to simultaneously continuing their failing antiretroviral therapy for 14 days. On day 15, those in the lenacapavir group began subcutaneous lenacapavir once every six months (26 weeks) in addition to an optimized background therapy. On day 15, the placebo group began oral lenacapavir plus an optimized background therapy for one week, then switched to subcutaneous lenacapavir once every six months.[3]
The primary efficacy endpoint was the percentage of patients that had a decrease in the HIV-1 viral load of at least 0.5log10 copies/ml by day 15. In the lenacapavir group, that endpoint was seen in 88% of the patients while in only 17% of the placebo group.[4] In Cohort 2, 36 subjects were given an optimized background regimen on day 1 along with oral lenacapavir on days 1,2, and 8, switching to subcutaneous lenacapavir once every six months (26 weeks) starting on day 15.
A secondary efficacy endpoint involved viral load. The endpoint was a viral load of less than 50 copies per/ml or a viral load of less than 200 copies per/ml. In cohort 1, at 26 weeks, a viral load of 50 copies per/ml was seen in 81% (29 of 36), and a viral load of less than 200 copies was seen in 89% (32 of 36).[4] In cohort 2, less than 50 copies per/ml was observed in 83% (30 of 36); and less than 200 copies in 86% (31 of 36).[4] The recent report in Lancet: HIV reports data at the 52-week point. At week 52, 83% (30 of 36) subjects in cohort 1 had HIV-1 RNA of less than 50 copies per mL, and 86% (31 of 36 ) had HIV-1 RNA of less than 200 copies per mL.[3] For cohort 2 at 52 weeks, 72% (26 of 36) had less than 50 copies per/ml, and 78% (28 of 36) had less than 200 copies per/ml.
 |
| Photo Source: European AIDS Treatment Group |
The overall theme is that the results at 52 weeks support the efficacy of lenacapavir injections every six months for those with multi-drug resistance to retrovirals. Consistent viral suppression was met, and therapeutic drug levels were maintained in the blood between injections. Most importantly, since lenacapavir is to be used with other medications, the injections do not increase pill burden or complicate daily regimens.
Although the results are promising, there are reasons to research much further before expanding lenacapavir for other uses, such as prevention. The cohort size was very small, at 72 participants. That is partly due to the requirements of the subjects. The participants had to have documented resistance to at least two drugs from at least three of the four major antiretroviral classes in addition to having advanced HIV disease. Additionally, while the data showed no significant safety issues, people living with HIV are known to have hypersensitivity issues with drug reactions. The CAPELLA clinical trial, along with CALIBRATE, a different lenacapavir clinical trial, together only have a total of 229 subjects.[5]
Much larger cohorts need to be examined in order to have comprehensive cross-sectional data to explore gender, age, and ethnicity differences. The complex variances of combination antiviral regimens of multi-drug resistant patients are also a significant concern. Once further lenacapavir research is conducted, the path of its utilization will be more apparent. It could even possibly become paired with another complete long-acting drug, creating an easy-to-use twice-yearly injection for all patients, whether multi-drug resistant or not.[5]
[1] Rivera, Viviana. (2023, September 1). FDA approves treatment for multi-drug resistant HIV. Retrieved from https://medicalxpress.com/news/2023-09-fda-treatment-multi-drug-resistant-hiv.html
[2] FDA Press Release (2022, December 22). FDA Approves New HIV Drug for Adults with Limited Treatment Options. Retrieved from https://www.fda.gov/news-events/press-announcements/fda-approves-new-hiv-drug-adults-limited-treatment-options
[3] Ogbuagu, O., Segal-Maurer, S., Ratanasuwan, W., Avihingsanon, A., Brinson, C., Workowski, K. A., Antinori, A., Yazdanpanah, Y., Trottier, B., Wang, H., Margot, N., Dvory-Sobol, H., Rhee, M. S., Baeten, J. M., Molina, J., DeJesus, E., Richmond, G., Berhe, M., Ruane, P., . . . Rassool, M. (2023). Efficacy and safety of the novel capsid inhibitor lenacapavir to treat multidrug-resistant HIV: week 52 results of a phase 2/3 trial. The Lancet HIV, 10(8), e497–e505. https://doi.org/10.1016/s2352-3018(23)00113-3
[4] Segal-Maurer, S., DeJesus, E., Stellbrink, H., Castagna, A., Richmond, G., Sinclair, G., Siripassorn, K., Ruane, P., Berhe, M., Wang, H., Margot, N., Dvory-Sobol, H., Hyland, R. H., Brainard, D. M., Rhee, M. S., Baeten, J. M., & Molina, J. (2022). Capsid Inhibition with Lenacapavir in Multidrug-Resistant HIV-1 Infection. The New England Journal of Medicine, 386(19), 1793–1803. https://doi.org/10.1056/nejmoa2115542
[5] SHarris, M. (2023). Lenacapavir: an attractive option, but proceed with caution. The Lancet HIV, 10(8), e486–e487. https://doi.org/10.1016/s2352-3018(23)00170-4
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.

No comments:
Post a Comment