On May 18th, an analysis of the AIDS Drug Assistance Program (ADAP) was released by the National Alliance of State & Territorial AIDS Directors (NASTAD). The 2017 National ADAP Monitoring Project Annual Report tracked state-by-state programmatic changes, emerging trends, and latest available data on the number of clients served, expenditures on prescription drugs, among other things.
On May 18th, an analysis of the AIDS Drug Assistance Program (ADAP) was released by the National Alliance of State & Territorial AIDS Directors (NASTAD). The 2017 National ADAP Monitoring Project Annual Report tracked state-by-state programmatic changes, emerging trends, and latest available data on the number of clients served, expenditures on prescription drugs, among other things.The report, which is published annually by NASTAD, provides stakeholders an important snapshot into ADAP-related data, information, and trends. This year's report focuses on several areas, including:
- The importance of the Ryan White Program and ADAP (p. 6)
- What does it take to achieve viral suppression (p. 20)
- Comprehensive care for people living with HIV/AIDS (p. 42)
- Who benefits from services (p. 58)
Upon releasing the 2017 National ADAP Monitoring Project Annual Report, Murray C. Penner, NASTAD's executive director, stated the following:[1]
"Over the course of time, there have been significant shifts in funding and client needs; ADAPs have worked to meet those needs, however, have sometimes found themselves unable to serve all those in need of services. Lessons have been learned from these circumstances and ADAPs continue to look to identify how they can meet client need and ensure program sustainability. At a time now when ADAPs are documenting program stability, it is imperative that ADAPs look back on how challenges were resolved and look to the future of client needs and determine ways to prepare for the future. ADAPs are at an unprecedented juncture of being able to look to target resources to populations that need them most, to partner with the RWPB to ensure that the whole client’s needs are met, and to identify ways to bolster treatment for individuals’ health."The 2017 National ADAP Monitoring Project Annual Report overall yielded some very compelling data on the success of the AIDS Drug Assistance Program nationwide in 2016. Some key points are:
- ADAPs provided medications to 225,517 clients in calendar year (CY) 2015, a 235% increase in utilization over the last 10 years;[2]
- The majority (77%) of all clients served by ADAPs in CY2015 were reported as virally suppressed, de ned as having a viral load that is less than or equal to 200 copies/mL;[3]
- Twenty-eight (28) states contribute funding to their ADAP budget.[4]
- Thirty-eight (38) states receive drug rebates to their ADAP budget.[5]
- Overall, nearly 98% of Part B and ADAP budgets are allocated to program services; only 2.2% of Part B and ADAP funding is used to administer the program;[6]
- The majority of ADAPs pay premiums (84%), deductibles (84%) and prescription co-payments/co-insurance (94%) on behalf of eligible clients.[7]
- Forty-three (43) ADAPs reported using funds for insurance purchasing/continuation, representing $161.8 million in estimated expenditures (10% of the ADAP budget at that time) for 30,621 ADAP clients, with an average cost per client of $5,284.[7]
 |
| Photo Source: NASTAD |
Several advocates commented on the 2017 National ADAP Monitoring Project Annual Report, providing some important state perspectives. They include:
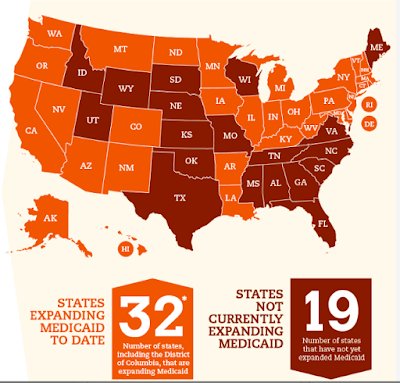
Ken Bargar, co-chair of the Florida HIV/AIDS Advocacy Network in Florida stated, "FHAAN has made access to our state's ADAP for Floridians a number one priority for many years. As Co Chair, I can tell you that we experience a great relationship with the Florida Department of Health, and we have provided many solutions for improving the program that they have implemented over the years. As a Medicaid non-expansion state, ADAP is crucial for people living with HIV in Florida. The increasing amount of clients receiving premium support for ACA plans has made this program robust and diverse in the ways they get access to HIV medication to our state’s most vulnerable clients. Recently, we were thrilled to see “pharmacy choice” finally became a reality for a section of the programs enrollees."
Eddie Hamilton, executive director of the ADAP Educational Initiative in Ohio, "In terms of transparency and the responsiveness to client’s concerns, Ohio's ADAP has come a long way since the last waiting list era. The ease of access to the program has drastically improved as there are now multiple routes of access (via case management, or direct application)."
Marcus J. Hopkins, an ADAP recipient and HIV/AIDS advocate in West Virginia, summarized, "West Virginia's ADAP is one of only twelve states in which 89% of enrolled clients in 2015 have achieved HIV Viral Loads ≤200. Our state had 1,139 clients in 2015, and only 3 Ryan White-specific clinics, meaning that many clients must travel 60 miles or more in order to reach one of these facilities. Our state is broken up into seven Ryan White regions, with 1 primary case manager contact per region. The small number of clinics serving 55 clinics (not including private Infectious Disease specialists) sometimes creates confusion, as clients living in different regions may have to coordinate between two different case workers. West Virginia's program also offers insurance continuation assistance, providing premium and co-pay assistance for clients enrolled in employer-based or ACA Insurance Marketplace coverage."
Matt Pagnotti, Director of Policy and Advocacy for AIDS Alabama, noted, "Since Alabama has failed to expand Medicaid under the ACA, the state's ADAP has operated as a vital safety net for thousands of people living with HIV in Alabama. Over three fourths of the clients served by Alabama's ADAP earn 133% FPL ($16,040 a year for a single adult) or less, most of whom find themselves in the "Medicaid coverage gap." In addition, roughly 16% of those served by ADAP in Alabama qualify for subsidized health insurance under the ACA marketplace. To assist these clients in overcoming financial barriers to access and create greater coverage completion, Alabama also operates an innovative Insurance Assistance Program that pays for premiums and co-payments."
The ADAP Advocacy Association commends NASTAD for its ongoing efforts to keep stakeholders informed, and engaged on the issues enumerated in this year's National ADAP Monitoring Project. Download a copy of the 2017 National ADAP Monitoring Project Annual Report.
__________
[1] Penner, Murray (2017, May 18); NASTAD Release: 2017 National ADAP Monitoring Project Annual Report; National Alliance of State & Territorial AIDS Directors.
[2] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 60. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[3] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 22. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[4] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 9. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[5] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 9. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[6] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 22. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[7] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 44. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[8] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 43. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[6] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 22. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[7] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 44. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.
[8] National Alliance of State & Territorial AIDS Directors (2017, May 18); 2017 National ADAP Monitoring Project Annual Report; p. 43. Retrieved from http://www.nastad.org/sites/default/files/2017-national-adap-monitoring-project-annual-report.pdf.