By: Jen Laws, Board Member, ADAP Advocacy Association, and HIV/transgender health advocate
The Biden Administration has repeatedly asserted a priority to achieving social equity by specifically addressing the systemic barriers to a freer, fairer society. Among one of the greatest barriers to equity is the financial burdens associated with complicated health conditions, an issue readily acknowledged by the administration’s special enrollment period (SEP) for the federal health care marketplace and expanded subsidies inclusion in the American Rescue Plan (ARP).
In reviewing this policy priority, the Biden Administration must consider the practical barriers created by burdensome application processes, particularly among programs aimed at helping the most marginalized and systemically disadvantaged among us. For people living with HIV/AIDS (PLWHAs), the eligibility recertification process for services under the Ryan White HIV/AIDS Program (RWHAP) – specifically in an effort to maintain medication access via AIDS Drug Assistance Programs (Part B) – is exceedingly burdensome. It represents a prime opportunity to reduce barriers to care. To that end, earlier this week the ADAP Advocacy Association called upon the Health Resources & Services Administration (HRSA) to improve the ADAP eligibility recertification process.
At current, in order for impoverished PLWHAs to access and maintain RWHAP-related benefits, they must first prove their HIV status, need based on other available benefits, and income upon applying for these benefits. Additionally, every six months thereafter, clients must prove their need based on other available benefits and income. For many states, this process includes multiple, required, in-person visits, verification of adherence to prescribed medication, verification of efforts toward seeking other public benefits, and verification of income. Some states allow for “self-attestation of no change” in terms of income and benefits.
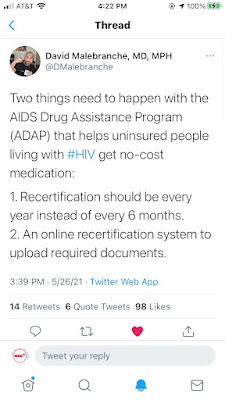
Dr. David Malebranche points out, this is an unnecessary and overly burdensome process not just for clients but for providers as well, “[It] makes my job difficult because often patients are given time with me that is sucked up by them having to see the benefits counselor, which throws a wrench in the entire clinic schedule and puts everything behind. It's bad for patient care and causes staff/provider burnout.”
 |
| Twitter - @DMalebranche |
(Screen capture, Twitter - @DMalebranche: "Two things need to happen with the AIDS Drug Assistance Program (ADAP) that helps uninsured people living with #HIV get no-cost medication: 1. Recertification should be every year instead of every 6 months. 2. An online recertification system to upload required documents.”)
Dr. Malebranche went further to describe how between patients and providers, paperwork burdens can be untraditional in the sense of having to access multiple portals or websites or produce paper documents. Lack of investment in supporting clinic resources, specifically in recruiting and retaining staffing talent among benefits and/or case managers, has left several of his clients either lacking reminders to begin recertification or late reminders – resulting in the client falling out of care. “That's just a few. Many of those issues can be tackled and improved, but people just don't want to on the local, state, and federal level.,” Dr. Malebranche continued, “And it just doesn’t follow the science. I have clients that don’t need to come see me every 6 months. Some of my clients don’t need to come in but once a year, if not for recertification.”
Indeed, the statutory requirement of ADAP grant recipients (states) and subrecipients does NOT include any specific time frame requirement for recertification. That policy is largely the result of an interpretation by HRSA through a “policy clarification notice” (PCN) for “[r]ecipients and their subrecipients are expected to vigorously pursue eligibility for other funding sources…”
Ultimately, HRSA decided this means states and their contractors providing RWHAP services must mask impoverished PLWHA to jump through exceeding challenging hoops every 6 months to prove their need and the help they need cannot be provided by anyone else. Absent that directive – which, again, has no statutory basis – HRSA has given little direction as to how states must verify the need of RWHAP services for PLWHA within the state. Instead, HRSA routinely provides other suggestions – lacking the strength of guidance - often responding to lamentation of PLWHA and subrecipients providing direct services about the burden of certain state processes.
In the wake of Covid-19 being declared a national public health emergency, HRSA issued further clarification to PCN 13-02, regarding processes related to eligibility for services under the RWHAP. Last updated on September 22, 2020, HRSA’s answer to all posted “frequently asked questions” regarding client recertification reads as follows:
"The health and safety of Ryan White HIV/AIDS Program (RWHAP) recipients, providers, and clients remains of paramount importance to HRSA during the COVID-19 pandemic. HRSA HAB encourages recipients to exercise flexibility in their eligibility determination and six-month recertification processes to promote social distancing practices and implement remote (telephonic or electronic) documentation processes when possible. Policy Clarification Notice (PCN) 13-02: Clarifications on Ryan White Program Client Eligibility Determinations and Recertification Requirements (PDF - 173 KB) outlines existing requirements and flexibilities with regard to RWHAP client eligibility determination and six-month recertification. Some examples of eligibility and recertification practices that are not required as per PCN 13-02 include:
- In-person actions related to eligibility
- Handwritten client signatures to accompany self-attestation
- Notarized documentation to support eligibility and recertification determination
- Documentation of any changes in income at six-month recertification if the change does not impact RWHAP eligibility
- Dis-enrolling clients from RWHAP services who are unable to recertify eligibility within a reasonable timeframe
RWHAP recipients and subrecipients assume the risk of recouping any RWHAP funds utilized for clients ultimately determined to be ineligible, and should instead charge an alternate payment source, or otherwise ensure that funds are returned to their RWHAP.
HRSA HAB encourages RWHAP recipients to reassess their organization's eligibility and recertification policies and procedures and remove any procedures that may impede social distancing or other public health strategies necessary to minimize Covid-19 transmission, or that impose any additional requirements beyond those specified in PCN 13-02."
In this, again, HRSA abdicates directing states to invest in making RWHAP services, and thus ADAPs, more meaningfully accessible to PLWHAs who need these services the most. In this particular area, the Biden Administration has an opportunity to both reduce barriers to care and prosperity for PLWHAs but to also change HRSA’s approach to modernization in a way that helps this administration achieve its goals in Ending the HIV Epidemic, domestically.
 |
| Photo Source: The Washington Free Beacon |
Dr. Malebranche agreed. “I shouldn’t have to hope a sample of antiretroviral medication will get a client through until their recertification finally gets seen. My clients shouldn’t have to worry more about the paperwork than getting their care and, frankly, that’s where we’re at. And we’re losing people to care because of it.” Dr. Malebranche said an ideal would be annual recertification, a single portal/website, and proper funding in order to fully staff the needs of a clinic, client, and reporting would go a long way to meeting the needs of the moment.
We need a uniform message between program operations, eligibility, and requirements and the message the Centers for Disease Control & Prevention, state health departments, and providers are supposed to be delivering: it’s time to meet people where they’re at. That means updating PCN 13-02 to allow for annual recertification and fund model program designs from the ground up. Answers to “FAQs” aren’t meaningful, if they lack enforcement and funding.
“I think now is a perfect time to revise things with ADAP. We've seen how the pandemic has disrupted care for people living with HIV, sexual and reproductive health and PrEP/PEP - why not make some modifications that have been needed for years now while we are having to make changes anyway?”
An analysis of the State ADAP recertification process is available online at https://tinyurl.com/ctf5t696.
Disclaimer: Guest blogs do not necessarily reflect the views of the ADAP Advocacy Association, but rather they provide a neutral platform whereby the author serves to promote open, honest discussion about public health-related issues and updates.
No comments:
Post a Comment