By: Brandon M. Macsata, CEO, ADAP Advocacy Association
On Monday, December 1st millions of football fans around the world were reminded of an important message during one of the most celebrated sports traditions on television: AIDS Activism is Alive in 2014!
Over 11 million viewers among the key 18-49 ratings demographic during the game saw Bank of America's (Red) TV Spot, 'One Step Closer,' featuring Bono. That number doesn't even reflect other demographics, or the number of people who have subsequently viewed the 30-second spot online.
Although the number of deaths in the United States, and elsewhere around the globe, has dramatically decreased with the advent of high-active anti-retroviral treatments (HAART) the need remains to educate people about HIV/AIDS. Bono states in the 'One Step Closer' spot that America has brought "this pandemic nearly to its knees." He is right, but all stakeholders in the fight against HIV/AIDS must re-commit themselves to this important struggle.
Some might argue that with the passage of the Affordable Care Act, or Obamacare, there is less cause for alarm because more people now have access to affordable health care. I disagree. There are emerging issues under the law that appear to disproportionately impact people living with long-term, chronic diseases such as HIV/AIDS. What played out with Blue Cross Blue Shield of Louisiana is evidence of what potentially lurks ahead. Fortunately for people living with HIV/AIDS, such as John East and others in Louisiana, organizations like Lambda Legal are fighting the good fight.
Medicaid expansion is important, but not the be-all, end-all solution. More and more doctors - especially specialty care physicians - are no longer accepting Medicaid assignment. The reimbursement rates are simply too low. That potentially leaves many patients with access to insurance, but they still cannot access the health care afforded to them. The uneven rollout of Medicaid expansion poses an entirely different set of issues.
The good news is there is still plenty of energy left in the fight against HIV/AIDS.
Even the ongoing debate over Pre-Exposure Prophylaxis, or PrEP, demonstrates that the passion within the HIV/AIDS community that once led to the Denver Principles is alive and well. Proponents and opponents of PrEP equally have sound arguments to support their respective positions. The community, however, should be mindful not to cut off its nose to spite its face, as the saying goes!
Today, we have new tools at our disposal that were unimaginable when the AIDS epidemic first appeared in the early 1980s. Wanda Brendle-Moss in North Carolina is leveraging Twitter (@WandaBrendleMos) every single day to spread the twin gospels of prevention and treatment. Patrick Ingram in Virginia and Aaron Laxton in Missouri are leveraging YouTube to educate people about HIV/AIDS. The Positive Women's Network (PWN), is unifying the voices of women impacted by this disease on a national level that serves as a model for self-advocacy.
HIV/AIDS might be down, but it certainly is not out for the count. Only by working together will be 'one step closer' to ending AIDS!
Editor's Note: This blog was originally published in the NeedyMeds December monthly newsletter.
This blog focuses on the federal commitment to fully fund the AIDS Drug Assistance Program (ADAP) for people living with HIV/AIDS.
Monday, December 22, 2014
Thursday, November 13, 2014
How does ADAP look under the Affordable Care Act?
By: Brandon M. Macsata, CEO, ADAP Advocacy Association
Over the last year, one of the most frequently asked questions by people living with HIV/AIDS, public policy advocates, representatives from the health care and pharmaceutical industries and others, "What is the future of the AIDS Drug Assistance Program now that the Affordable Care Act is law?"
The answer is simple: It is too early to know for certain!
At first glance, data trends suggest that the passage of the ACA and its subsequent implementation has not slowed down client enrollment in ADAPs nationwide. According to the "National ADAP Monitoring Project - Annual Report," published by the National Alliance of State & Territorial AIDS Directors (NASTAD), client enrollment increased by over 15,000 between 2012 and 2013, or about an 8% increase. Last year, over 210,000 people living with HIV/AIDS were enrolled in ADAP. [1]
Not surprisingly, California has the largest statewide enrollment, with 22,702 clients, followed by New York with 17,193 clients, and Florida with 14,058 clients. Over sixty percent (97,142 clients) of the total clients served by ADAP were served by the top ten states -- including Texas, Puerto Rico, Illinois, North Carolina, Georgia, New Jersey and Pennsylvania). [2]
One of the consistent themes heard at our 2014 Summit ("Intersection between ACA & ADAP") and 2014 Annual Conference ("Future of the AIDS Drug Assistance Program") was without concrete data, it is premature to make any assumptions about the Ryan White CARE Act, in general, and the AIDS Drug Assistance Programs, specifically. Another message that was fairly consistent, there is a significant disconnect between the advocacy work being done on Capitol Hill and the boots on the ground in local communities. It is also ill-advised to open-up the Ryan White law until we can better evaluate the intersection with the ACA, as well as the future of ADAP!
Clearly, ADAPs will remain a vital safety net for thousands of people living with HIV/AIDS next year and into the foreseeable future.
Probably one of the biggest unknown variables is the ongoing Medicaid expansion. "Spotty" is probably the best word to describe whether states are exercising the option to expand their Medicaid programs. Not surprisingly, some of the most resistance has come from southern states controlled by Republican Governors, or Republican State Legislatures.
To check out the most up-to-date information about state-by-state efforts to expand Medicaid, visit http://www.advisory.com/daily-briefing/resources/primers/medicaidmap.
Another added variable is the recent Republican electoral wave. Whereas some pragmatic Republican legislators have moved beyond the "Repeal & Replace" chatter about Obamacare, there remain plenty of hard-liners who wish to do away with the law, or at least strip it of some major provisions. It is clearly too early to tell, but President Obama's veto pen is probably the law's best defense.
The ACA is also fueling new challenges for people living with HIV/AIDS; among them, emerging discriminatory practices. Monitoring these trends is an essential responsibility for all ADAP stakeholders. (Editor's Note: CLICK HERE to register for a free webinar, "Update on ACA Discriminatory Marketplace Exchange Practices")
One thing is abundantly clear in this conversation, and that is nothing is clear whatsoever. There are so many moving parts that could potentially impact the access to care for people living with HIV/AIDS.
_________
[1] NASTAD, National ADAP Monitoring Project Annual Report, February 2014, Chart 10, Page 13.
[2] NASTAD National ADAP Monitoring Project Annual Report - February 2014, Chart 12, Page 14.
Over the last year, one of the most frequently asked questions by people living with HIV/AIDS, public policy advocates, representatives from the health care and pharmaceutical industries and others, "What is the future of the AIDS Drug Assistance Program now that the Affordable Care Act is law?"
The answer is simple: It is too early to know for certain!
At first glance, data trends suggest that the passage of the ACA and its subsequent implementation has not slowed down client enrollment in ADAPs nationwide. According to the "National ADAP Monitoring Project - Annual Report," published by the National Alliance of State & Territorial AIDS Directors (NASTAD), client enrollment increased by over 15,000 between 2012 and 2013, or about an 8% increase. Last year, over 210,000 people living with HIV/AIDS were enrolled in ADAP. [1]
 |
| Chart: ADAP Client Enrollment, June 2003-2013 |
Not surprisingly, California has the largest statewide enrollment, with 22,702 clients, followed by New York with 17,193 clients, and Florida with 14,058 clients. Over sixty percent (97,142 clients) of the total clients served by ADAP were served by the top ten states -- including Texas, Puerto Rico, Illinois, North Carolina, Georgia, New Jersey and Pennsylvania). [2]
 |
| Chart: ADAP Clients Served and Top Ten States, by Clients Served, June 2013 |
One of the consistent themes heard at our 2014 Summit ("Intersection between ACA & ADAP") and 2014 Annual Conference ("Future of the AIDS Drug Assistance Program") was without concrete data, it is premature to make any assumptions about the Ryan White CARE Act, in general, and the AIDS Drug Assistance Programs, specifically. Another message that was fairly consistent, there is a significant disconnect between the advocacy work being done on Capitol Hill and the boots on the ground in local communities. It is also ill-advised to open-up the Ryan White law until we can better evaluate the intersection with the ACA, as well as the future of ADAP!
Clearly, ADAPs will remain a vital safety net for thousands of people living with HIV/AIDS next year and into the foreseeable future.
Probably one of the biggest unknown variables is the ongoing Medicaid expansion. "Spotty" is probably the best word to describe whether states are exercising the option to expand their Medicaid programs. Not surprisingly, some of the most resistance has come from southern states controlled by Republican Governors, or Republican State Legislatures.
 |
| Where the States Stand on Medicaid Expansion |
Another added variable is the recent Republican electoral wave. Whereas some pragmatic Republican legislators have moved beyond the "Repeal & Replace" chatter about Obamacare, there remain plenty of hard-liners who wish to do away with the law, or at least strip it of some major provisions. It is clearly too early to tell, but President Obama's veto pen is probably the law's best defense.
The ACA is also fueling new challenges for people living with HIV/AIDS; among them, emerging discriminatory practices. Monitoring these trends is an essential responsibility for all ADAP stakeholders. (Editor's Note: CLICK HERE to register for a free webinar, "Update on ACA Discriminatory Marketplace Exchange Practices")
One thing is abundantly clear in this conversation, and that is nothing is clear whatsoever. There are so many moving parts that could potentially impact the access to care for people living with HIV/AIDS.
_________
[1] NASTAD, National ADAP Monitoring Project Annual Report, February 2014, Chart 10, Page 13.
[2] NASTAD National ADAP Monitoring Project Annual Report - February 2014, Chart 12, Page 14.
Thursday, October 30, 2014
Black Market HIV/AIDS Medications
By: Jim Dahl, Board Member, Partnership for Safe Medicines (PSM)
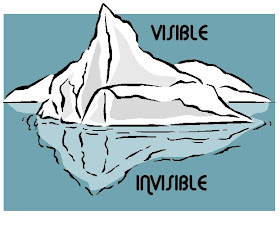
Almost since there were HIV/AIDS treatments, unlicensed distributors have been selling dangerous black market medications to American pharmacies, unscrupulous secondary wholesale distributors, and patients. Since 2006 at least 86 individuals have been charged with distributing HIV and AIDS medicines in the United States. These cases are just the tip of the iceberg.
The United States has the safest drug supply in the world. The FDA and licensing programs in individual states ensure that every entity in the American drug supply chain is answerable to a regulator. Companies that sell drugs outside of the FDA-approved drug supply are not accountable to the FDA, state licensing boards or anyone. Counterfeiters substitute cheap ingredients, offer medicines in unfamiliar doses and omit instructions and safety warnings. Their medicine may contain harmful chemicals or contaminants; it may contain no active ingredients at all. Counterfeiters are canny marketers. Their websites are very convincing, but they sell medicines that may be expired, contaminated, diluted or damaged during shipping. Patients who buy these drugs risk taking substandard medicines, and substandard medicines lead to higher viral loads, poor health and drug resistance, even if patients are conscientious about their drug regimen.
These aren't hypothetical risks.
In 2000, university professor Rick Roberts learned that the Serostim he had been taking to treat HIV wasting syndrome was counterfeit. The fake Serostim had made its way to his pharmacy via unlicensed distributors that had forged documentation to make it look legitimate. Roberts eventually recovered his health, but one child—a brain cancer survivor—suffered developmental and growth delays after being treated with another growth hormone being sold by these groups.
Since 2012, investigators have uncovered diversion of HIV/AIDS medicines on a massive scale. Customers of New York branches of MOMS Pharmacy were prescribed $274 million in second hand, stolen or expired HIV treatments. The FBI seized more than 33,000 bottles of second hand AIDS, asthma and schizophrenia drugs and 250,000 loose pills from drug diverters in New York. A Texas-based company called Cumberland Distribution sold $58 million in HIV/AIDS, antipsychotics and diabetes treatments to pharmacies. Their sources had acquired the drugs from “street level drug diverters.”
In late 2005 after just retiring as Assistant Director of FDA’s Office of Criminal Investigation (OCI), I testified before a House Subcommittee that in my time at the agency I hadn’t seen a counterfeit drug get into the otherwise legitimate supply chain without the aid of a pre-existing diversion infrastructure. I’m confident the same can be said today. Diverted drugs are not only unreliable but drug diversion poses an additional risk. Addicts who resell their medication are often selling vials they have already used. It is standard practice to take a dose of an IV drug and replace the missing contents with water using the same syringe. As many as 30,000 have been exposed to hepatitis C as a result of diversion in hospital settings since 2004; who knows what the exposure rate has been from black market injectables?
In the face of this threat, we must give patients the tools to be safe.
Patients need strategies to save money safely. Counsel them to adopt generics when they are appropriate. Let them know that they can comparison shop online for the lowest prices for safe, licensed online pharmacies at Pharmahelper.com and compare prices at their neighborhood pharmacies on websites such as WeRx.com, LowestMeds.com and GoodRX.com. If they are un- or under-insured, be sure they know about cards like the NeedyMeds Drug Discount Card, and direct them to prescription assistance program resources at NeedyMeds and the Partnership for Prescription Assistance.
Patients need to know how to spot questionable drugs. In medical settings, they should examine drug packaging to verify that it is in good condition and that its labeling is accurate and in English, and keep a record of the medicine lot number. At home, they should verify that their medicine's packaging is clean and correctly sealed, with instructions in English, and that new medication has the same packaging as past medication, with no differences in paper, printing, color or fonts. Patients should also examine the appearance of medicine; if it looks chipped or cracked, or different from earlier prescriptions, it may be fake.
Finally, patients and medical professionals should be alert to the possibility that a patient's treatment may not be working because the medication itself is compromised. Changes to the way a medicine tastes, new side effects or adverse effects and failure of treatment might signal changes to a drug.
If there's any question about whether a drug is counterfeit, patients should contact the pharmacy where they purchased their medicine. Patients and medical professionals can contact the FDA and the manufacturer of the medication to report concerns. The FDA can be contacted by calling toll-free 1-800-FDA-1088 (800-332-1088), or on the Web at www.fda.gov/medwatch.
Almost since there were HIV/AIDS treatments, unlicensed distributors have been selling dangerous black market medications to American pharmacies, unscrupulous secondary wholesale distributors, and patients. Since 2006 at least 86 individuals have been charged with distributing HIV and AIDS medicines in the United States. These cases are just the tip of the iceberg.
The United States has the safest drug supply in the world. The FDA and licensing programs in individual states ensure that every entity in the American drug supply chain is answerable to a regulator. Companies that sell drugs outside of the FDA-approved drug supply are not accountable to the FDA, state licensing boards or anyone. Counterfeiters substitute cheap ingredients, offer medicines in unfamiliar doses and omit instructions and safety warnings. Their medicine may contain harmful chemicals or contaminants; it may contain no active ingredients at all. Counterfeiters are canny marketers. Their websites are very convincing, but they sell medicines that may be expired, contaminated, diluted or damaged during shipping. Patients who buy these drugs risk taking substandard medicines, and substandard medicines lead to higher viral loads, poor health and drug resistance, even if patients are conscientious about their drug regimen.
These aren't hypothetical risks.
In 2000, university professor Rick Roberts learned that the Serostim he had been taking to treat HIV wasting syndrome was counterfeit. The fake Serostim had made its way to his pharmacy via unlicensed distributors that had forged documentation to make it look legitimate. Roberts eventually recovered his health, but one child—a brain cancer survivor—suffered developmental and growth delays after being treated with another growth hormone being sold by these groups.
Since 2012, investigators have uncovered diversion of HIV/AIDS medicines on a massive scale. Customers of New York branches of MOMS Pharmacy were prescribed $274 million in second hand, stolen or expired HIV treatments. The FBI seized more than 33,000 bottles of second hand AIDS, asthma and schizophrenia drugs and 250,000 loose pills from drug diverters in New York. A Texas-based company called Cumberland Distribution sold $58 million in HIV/AIDS, antipsychotics and diabetes treatments to pharmacies. Their sources had acquired the drugs from “street level drug diverters.”
In late 2005 after just retiring as Assistant Director of FDA’s Office of Criminal Investigation (OCI), I testified before a House Subcommittee that in my time at the agency I hadn’t seen a counterfeit drug get into the otherwise legitimate supply chain without the aid of a pre-existing diversion infrastructure. I’m confident the same can be said today. Diverted drugs are not only unreliable but drug diversion poses an additional risk. Addicts who resell their medication are often selling vials they have already used. It is standard practice to take a dose of an IV drug and replace the missing contents with water using the same syringe. As many as 30,000 have been exposed to hepatitis C as a result of diversion in hospital settings since 2004; who knows what the exposure rate has been from black market injectables?
In the face of this threat, we must give patients the tools to be safe.
Patients need strategies to save money safely. Counsel them to adopt generics when they are appropriate. Let them know that they can comparison shop online for the lowest prices for safe, licensed online pharmacies at Pharmahelper.com and compare prices at their neighborhood pharmacies on websites such as WeRx.com, LowestMeds.com and GoodRX.com. If they are un- or under-insured, be sure they know about cards like the NeedyMeds Drug Discount Card, and direct them to prescription assistance program resources at NeedyMeds and the Partnership for Prescription Assistance.
Patients need to know how to spot questionable drugs. In medical settings, they should examine drug packaging to verify that it is in good condition and that its labeling is accurate and in English, and keep a record of the medicine lot number. At home, they should verify that their medicine's packaging is clean and correctly sealed, with instructions in English, and that new medication has the same packaging as past medication, with no differences in paper, printing, color or fonts. Patients should also examine the appearance of medicine; if it looks chipped or cracked, or different from earlier prescriptions, it may be fake.
Finally, patients and medical professionals should be alert to the possibility that a patient's treatment may not be working because the medication itself is compromised. Changes to the way a medicine tastes, new side effects or adverse effects and failure of treatment might signal changes to a drug.
If there's any question about whether a drug is counterfeit, patients should contact the pharmacy where they purchased their medicine. Patients and medical professionals can contact the FDA and the manufacturer of the medication to report concerns. The FDA can be contacted by calling toll-free 1-800-FDA-1088 (800-332-1088), or on the Web at www.fda.gov/medwatch.
Thursday, October 2, 2014
The Difficulty in Scoring Gridlock
By: Brandon M. Macsata, CEO, ADAP Advocacy Association
The ADAP Advocacy Association (aaa+) has published its annual Congressional Scorecard between 2009--2012, evaluating Members of Congress on their support of the AIDS Drug Assistance Programs (ADAP). The 2012 Scorecard, however, will be the last published ranking on congressional activity.
Why?
| Source: ASPA National Weblog |
Simply put: it is too difficult to score gridlock. There was a time that the two major political parties could hold serious policy disagreements on the issues facing the nation...including on HIV/AIDS. Unfortunately that is no longer the case.
Whether it is Republicans controlling the majority (as in the U.S. House of Representatives), or the Democrats in the U.S. Senate, policy disagreements have succumb to political posturing. BOTH sides are equally to blame, and anyone suggesting otherwise is simply blinded by personal politics. The (legitimate) news media, establishment political class, and the general public all agree on this point.
There are 34 days until the upcoming midterm congressional elections, but it is obvious that the next election will immediately begin hours after the votes are cast this year...regardless of the outcome. Therein lies the true problem, nothing is getting done in Washington because both the Republicans and Democrats are more worried about public polling polls, focus group results and the potential backlash from making tough decisions. Things only appear to be getting worse, too!
Whereas programs like the Ryan White CARE Act--which includes ADAP--continue to enjoy strong bipartisan support, it is overshadowed by the ongoing broader cantankerous debate over the Affordable Care Act, or Obamacare. One political party insists that it will be the end of the Republic (even one potential presidential candidate had the audacity to say it is worse than slavery, the Holocaust and 9/11). The other political party has completely buried its collective head in the sand trying to ignore the emerging...and very real...unintended consequences surrounding the law. There is no middle ground, it seems.
When the ADAP Advocacy Association's Congressional Scorecard was initially published, it proved to be an important tool...among many others...to help educate patients on how the nation's leaders were addressing HIV/AIDS in this country. Many people living with HIV/AIDS and policy advocates applauded the report card because it helped them to make informed decisions. But now there is no leadership on Capitol Hill.
That's not to say that there aren't congressional leaders in the fight against HIV/AIDS!!! Quite the contrary. The Congressional HIV/AIDS Caucus--under the leadership of Rep. Barbara Lee (D-CA), Rep. Jim McDermott (D-WA) and Rep. Ileana Ros-Lehtinen (R-FL)--has assembled over 70 Members of Congress to ensure that HIV/AIDS issues remain on the table. Their bipartisan commitment to the fight against HIV/AIDS is unquestionable.
To learn more about the Congressional HIV/AIDS Caucus, go to http://hivaidscaucus-lee.house.gov.
Thursday, September 11, 2014
Shifting Landscape of HIV Housing & its Impact on Healthcare
By: Brandon M. Macsata, CEO, ADAP Advocacy Association
For people living with HIV/AIDS, there is probably only one thing that is more important to them than access to affordable healthcare and treatment: housing. But like healthcare, housing has to be affordable otherwise it provides little relief for the people who are trying to manage the chronic nature of their condition.
In 2012, Priced Out in 2012 -- which was released by the Technical Assistance Collaborative (TAC) and the CCD Housing Task Force -- documents how affordable housing is often unattainable for people with disabilities, including people living with HIV/AIDS. The report concluded, "...non-elderly adults with disabilities living on Social Security Income confront an enormous housing affordability gap across the entire nation."
Whereas Priced Out in 2012 focused on the U.S. Department of Housing & Urban Development's (HUD) Section 811 program, there exists sufficient parallel with HUD's Housing Opportunities for People with AIDS (HOPWA) program. HOPWA is the only Federal program dedicated to the housing needs of people living with HIV/AIDS, benefiting low-income persons living with HIV/AIDS and their families. [1]
Affordable housing may be the most important factor for successful medical outcomes for those living with HIV/AIDS. To that end, HOPWA is a critical program to help people living with HIV/AIDS with stable affordable housing that isn’t available in mainstream housing programs.
The Obama administration has proposed significant changes in the HOPWA legislation. Additionally, there are plans by HUD to move the HIV/AIDS housing office under the umbrella of the massive homeless programs. Those proposed changes have been met with some concern, but even more unanswered questions by stakeholders about the impact on people living with HIV/AIDS.
In response, HUD issued the following statement:
"The Department’s FY 2015 HOPWA congressional budget justification includes a legislative proposal to change the formula and to expand the provision of short-term housing assistance. Congressional action is required prior to enactment of the proposal, as the HOPWA statute must be amended to enable the use of living HIV cases. This is due to the existing statutory language referring only to cumulative AIDS cases for purposes of providing formula grant awards. As such, the purpose of this notification to dispel any misunderstanding regarding the status of this legislative request since it remains a proposed action. In fact, the Department has previously submitted the legislative request in the FY 2013 and FY 2014 HOPWA budget requests without congressional action." [2]
A coalition of housing organizations have been closely monitoring the HOPWA Modernization proposal, including the National AIDS Housing Coalition (NAHC), Southern AIDS Coalition, Housing Works, AIDS Alabama, HIV Prevention Justice Alliance, and many others. These organizations have convened meetings, hosted workshops and gathered important community input.
As part of the ADAP Advocacy Association's ongoing commitment to the principles of the Housing is Healthcare, ADAP stakeholders are encouraged to register for its free webinar: Shifting Landscape of HIV Housing & its Impact on Healthcare. The webinar, which will be held on Thursday, October 23rd, is FREE to all stakeholders.
This webinar will explain the proposed changes and how they will impact people living with HIV/AIDS who need housing, including how it might undermine the Housing is Healthcare paradigm.
CLICK HERE to register for the webinar, Shifting Landscape of HIV Housing & its Impact on Healthcare.
[1] U.S. Department of Housing & Urban Development. HUD Exchange. Housing Opportunities for People with AIDS. 2014.
[2] U.S. Department of Housing & Urban Development. HUD Exchange. Update on the Status of the Proposed HOPWA Formula Change. June 23, 2014.
For people living with HIV/AIDS, there is probably only one thing that is more important to them than access to affordable healthcare and treatment: housing. But like healthcare, housing has to be affordable otherwise it provides little relief for the people who are trying to manage the chronic nature of their condition.
In 2012, Priced Out in 2012 -- which was released by the Technical Assistance Collaborative (TAC) and the CCD Housing Task Force -- documents how affordable housing is often unattainable for people with disabilities, including people living with HIV/AIDS. The report concluded, "...non-elderly adults with disabilities living on Social Security Income confront an enormous housing affordability gap across the entire nation."
Whereas Priced Out in 2012 focused on the U.S. Department of Housing & Urban Development's (HUD) Section 811 program, there exists sufficient parallel with HUD's Housing Opportunities for People with AIDS (HOPWA) program. HOPWA is the only Federal program dedicated to the housing needs of people living with HIV/AIDS, benefiting low-income persons living with HIV/AIDS and their families. [1]
Affordable housing may be the most important factor for successful medical outcomes for those living with HIV/AIDS. To that end, HOPWA is a critical program to help people living with HIV/AIDS with stable affordable housing that isn’t available in mainstream housing programs.
The Obama administration has proposed significant changes in the HOPWA legislation. Additionally, there are plans by HUD to move the HIV/AIDS housing office under the umbrella of the massive homeless programs. Those proposed changes have been met with some concern, but even more unanswered questions by stakeholders about the impact on people living with HIV/AIDS.
In response, HUD issued the following statement:
"The Department’s FY 2015 HOPWA congressional budget justification includes a legislative proposal to change the formula and to expand the provision of short-term housing assistance. Congressional action is required prior to enactment of the proposal, as the HOPWA statute must be amended to enable the use of living HIV cases. This is due to the existing statutory language referring only to cumulative AIDS cases for purposes of providing formula grant awards. As such, the purpose of this notification to dispel any misunderstanding regarding the status of this legislative request since it remains a proposed action. In fact, the Department has previously submitted the legislative request in the FY 2013 and FY 2014 HOPWA budget requests without congressional action." [2]
A coalition of housing organizations have been closely monitoring the HOPWA Modernization proposal, including the National AIDS Housing Coalition (NAHC), Southern AIDS Coalition, Housing Works, AIDS Alabama, HIV Prevention Justice Alliance, and many others. These organizations have convened meetings, hosted workshops and gathered important community input.
As part of the ADAP Advocacy Association's ongoing commitment to the principles of the Housing is Healthcare, ADAP stakeholders are encouraged to register for its free webinar: Shifting Landscape of HIV Housing & its Impact on Healthcare. The webinar, which will be held on Thursday, October 23rd, is FREE to all stakeholders.
This webinar will explain the proposed changes and how they will impact people living with HIV/AIDS who need housing, including how it might undermine the Housing is Healthcare paradigm.
CLICK HERE to register for the webinar, Shifting Landscape of HIV Housing & its Impact on Healthcare.
[1] U.S. Department of Housing & Urban Development. HUD Exchange. Housing Opportunities for People with AIDS. 2014.
[2] U.S. Department of Housing & Urban Development. HUD Exchange. Update on the Status of the Proposed HOPWA Formula Change. June 23, 2014.
Friday, August 8, 2014
The ADAP Directory Puts the Right People in Control: PATIENTS
Newly diagnosed with HIV-infection, and need assistance with your medications?
Already living with HIV/AIDS, and thinking about moving to another state but uncertain if you'll lose your medication assistance?
Recently unemployed or lost your health insurance coverage, and need assistance for your HIV medications?
There is a new tool to help patients living with HIV/AIDS learn more about the AIDS Drug Assistance Program (ADAP), which exists in all 50 U.S. States and the 6 U.S. Territories. The tool puts patients in control of their own healthcare decisions.
The ADAP Advocacy Association launched its comprehensive ADAP Directory earlier this week at the opening ceremony of its 7th Annual Conference in Washington, DC. The ADAP Directory is its groundbreaking flagship program, made possible by generous support from AbbVie, Merck, and Walgreens.
The ADAP Directory is a new, innovative approach to ensure people living with HIV-infection have access to the information and resources they need to live healthy and productive lives. The ADAP Directory consolidates useful ADAP-related information from all 50 states and 6 territories into one convenient location for:
• Easy access to ADAP resources organized by state and territory;
• Updated, current information for all 56 state ADAPs; and
• Uniform presentation of ADAP information for effective advocacy and easy dissemination.
The “Perfect Storm” that had befallen the cash-strapped ADAPs exposed some very real deficiencies in the amount and quality of information made readily available to patients living with HIV/AIDS. As of July 28th, ADAP waiting lists still existed in one state, with 35 people in Utah being denied access to care and treatment.
While these numbers are nowhere near as high as they were during the last ADAP crisis, they still demonstrate the need for better linkages to care. In addition, these numbers don’t even accurately reflect the scope of the crisis, because hundreds more have been dis-enrolled and there have been numerous other cost containment measures adopted that all have resulted in restricted access to care – including capped enrollment, reduced formularies, implemented medical criteria, instituted monthly expenditure cap, discontinued reimbursement of laboratory assays, instituted annual expenditure cap, and instituted client cost-sharing
"As woman living out loud with HIV/AIDS, and an awesomely proud member North Carolina's ADAP advocacy community, I firmly support the ADAP Directory because it is long-overdue," summarized Wanda Brendle-Moss, who received the ADAP Advocacy Association's "ADAP Emerging Leader of the Year Award. "It is an ADAP advocacy dream tool!"
There currently exists only a “patch-work” of relevant information accessible to patients, so the ADAP Directory is a groundbreaking initiative. It serves a one-stop online resource center to assist social workers, patient advocates and medical practitioners – but more importantly, it will provide patients with the necessary resources and tools to become more active decision-makers with their care.
“The ADAP Directory puts patients in the driver’s seat by linking them to the relevant information about all 56 ADAPs, as well as useful resources and tools,” stated Brandon Macsata, CEO of the ADAP Advocacy Association. “Patients deserve new, innovative approaches to linking them to the information, resources, medical care and the treatment options that will keep them healthy, productive members in their communities.”
Learn more about the ADAP Directory: http://adap.directory/
Already living with HIV/AIDS, and thinking about moving to another state but uncertain if you'll lose your medication assistance?
Recently unemployed or lost your health insurance coverage, and need assistance for your HIV medications?
There is a new tool to help patients living with HIV/AIDS learn more about the AIDS Drug Assistance Program (ADAP), which exists in all 50 U.S. States and the 6 U.S. Territories. The tool puts patients in control of their own healthcare decisions.
The ADAP Advocacy Association launched its comprehensive ADAP Directory earlier this week at the opening ceremony of its 7th Annual Conference in Washington, DC. The ADAP Directory is its groundbreaking flagship program, made possible by generous support from AbbVie, Merck, and Walgreens.
The ADAP Directory is a new, innovative approach to ensure people living with HIV-infection have access to the information and resources they need to live healthy and productive lives. The ADAP Directory consolidates useful ADAP-related information from all 50 states and 6 territories into one convenient location for:
• Easy access to ADAP resources organized by state and territory;
• Updated, current information for all 56 state ADAPs; and
• Uniform presentation of ADAP information for effective advocacy and easy dissemination.
While these numbers are nowhere near as high as they were during the last ADAP crisis, they still demonstrate the need for better linkages to care. In addition, these numbers don’t even accurately reflect the scope of the crisis, because hundreds more have been dis-enrolled and there have been numerous other cost containment measures adopted that all have resulted in restricted access to care – including capped enrollment, reduced formularies, implemented medical criteria, instituted monthly expenditure cap, discontinued reimbursement of laboratory assays, instituted annual expenditure cap, and instituted client cost-sharing
"As woman living out loud with HIV/AIDS, and an awesomely proud member North Carolina's ADAP advocacy community, I firmly support the ADAP Directory because it is long-overdue," summarized Wanda Brendle-Moss, who received the ADAP Advocacy Association's "ADAP Emerging Leader of the Year Award. "It is an ADAP advocacy dream tool!"
There currently exists only a “patch-work” of relevant information accessible to patients, so the ADAP Directory is a groundbreaking initiative. It serves a one-stop online resource center to assist social workers, patient advocates and medical practitioners – but more importantly, it will provide patients with the necessary resources and tools to become more active decision-makers with their care.
“The ADAP Directory puts patients in the driver’s seat by linking them to the relevant information about all 56 ADAPs, as well as useful resources and tools,” stated Brandon Macsata, CEO of the ADAP Advocacy Association. “Patients deserve new, innovative approaches to linking them to the information, resources, medical care and the treatment options that will keep them healthy, productive members in their communities.”
Learn more about the ADAP Directory: http://adap.directory/
Thursday, July 17, 2014
ADAP Cost Containment Measures Undermine Patient Care
According to the National Alliance of State & Territorial AIDS Directors (NASTAD) and its most recent ADAP Watch, there are ten State AIDS Drug Assistance Programs (ADAPs) with cost-containment measures in place since April 1, 2013 (reported as of April 7, 2014). More cost-containment measures might be coming, too. For patients, these cost containment measures amount to being denied access to timely, appropriate health care. Nothing more; nothing less!
During the "Perfect Storm" that besieged ADAPs nationwide between 2008-2013, especially in the southern states, most of the HIV/AIDS advocacy community concentrated on eliminating the record high waiting lists. At their peak, ADAP waiting lists reached approximately 10,000 patients across a dozen states. Whereas at the time the dilemma was certainly embarrassing for states like Florida...which witnessed its program basically fall apart...it galvanized the HIV/AIDS advocacy community.
National leadership was spearheaded by AIDS Healthcare Foundation, Housing Works, NASTAD, Community Access National Network, The AIDS Institute, HealthHIV, and many, many other organizations. The national efforts were surpassed by the advocacy efforts at the state level, including notable grassroots advocacy led by AIDS Alabama, Florida HIV/AIDS Advocacy Network (FHAAN), AIDS Foundation of Chicago and Georgia Equality, just to name a few.
Even though that collective leadership paid off, evidenced by ADAP waiting lists being down to 12 individuals in one state (Utah), it is still needed today. It is needed to eliminate the remaining cost containment measures.
Reduced drug formularies, restricted financial eligibility, monthly expenditure caps and cost-sharing are only some of the cost containment measures, but they're equally as dangerous as ADAP waiting lists. The ADAP Advocacy Association warned about the "tip of the iceberg" and that warning remains today!
These remaining ADAP cost containment measures undermine patient care, and the HIV/AIDS advocacy community must vigilant to ensure that every patient is afforded access to health care.
During the "Perfect Storm" that besieged ADAPs nationwide between 2008-2013, especially in the southern states, most of the HIV/AIDS advocacy community concentrated on eliminating the record high waiting lists. At their peak, ADAP waiting lists reached approximately 10,000 patients across a dozen states. Whereas at the time the dilemma was certainly embarrassing for states like Florida...which witnessed its program basically fall apart...it galvanized the HIV/AIDS advocacy community.
National leadership was spearheaded by AIDS Healthcare Foundation, Housing Works, NASTAD, Community Access National Network, The AIDS Institute, HealthHIV, and many, many other organizations. The national efforts were surpassed by the advocacy efforts at the state level, including notable grassroots advocacy led by AIDS Alabama, Florida HIV/AIDS Advocacy Network (FHAAN), AIDS Foundation of Chicago and Georgia Equality, just to name a few.
Even though that collective leadership paid off, evidenced by ADAP waiting lists being down to 12 individuals in one state (Utah), it is still needed today. It is needed to eliminate the remaining cost containment measures.
Reduced drug formularies, restricted financial eligibility, monthly expenditure caps and cost-sharing are only some of the cost containment measures, but they're equally as dangerous as ADAP waiting lists. The ADAP Advocacy Association warned about the "tip of the iceberg" and that warning remains today!
These remaining ADAP cost containment measures undermine patient care, and the HIV/AIDS advocacy community must vigilant to ensure that every patient is afforded access to health care.
Wednesday, June 25, 2014
Never Miss a Dose: The Vital Importance of Treatment When You Have HIV-Infection
By Leslie Vandever, guest blogger
Your body’s tough. Its immune system produces protective T (thymus) cells to fight off infection by viruses, bacteria, and other foreign invaders from outside. Your T-cells step up and squash these malicious invaders before they can wreak havoc and make you sick.
But the human immunodeficiency virus, or HIV, specifically goes after and kills T-cells. In time, it kills off so many that there aren’t enough left to fight off the usual infections and diseases we’re all exposed to every day. The result is AIDS—acquired immunodeficiency syndrome.
When you have AIDS, you can get very sick, very quickly. Overcoming each illness requires monumental effort, and each battle leaves your body weaker. Eventually, one or more diseases or infections take over. Weakened and unable to fight back, you’ll die.
That’s the bleak truth about HIV/AIDS. But it doesn’t have to be that way.
So far, medical science hasn’t been able to find a cure for HIV, but antiretroviral treatments (ARVs) inhibit the virus in a number of ways, including its ability to reproduce. ARVs keep your “viral load” under control and your T-cells numerous enough to protect you from other viruses and diseases.
And that’s why it’s so important for you to take your HIV medications exactly as prescribed. Even a single missed dose can allow HIV to replicate and function better, making it that much harder for the ARV to bring it back under control. If you periodically skip doses or stop taking the medication temporarily, you’re setting your body up for AIDS.
Medication non-compliance is a well-known, widespread problem.
Missing medication doses or messing them up can happen to anyone, not just patients living with HIV-infection. Sometimes taking a dose is inconvenient—we’re not near a water source, or we’re otherwise occupied at the time we should be taking them and then forget to take them later. We’re all human. It happens.
Other reasons for ARV non-compliance are more complicated—and potentially more serious. According to a paper published in the peer-reviewed journal LGBT Health, mental health issues like depression, and substance abuse—particularly alcohol and crystal methamphetamine—are prevalent among gay, LGBT, bisexual and other men who have sex with men (MSM). They can have a profound and disastrous effect on an individual’s ability to stick to ARVs.
Just getting through each day can be a huge challenge if you’re suffering from depression, anxiety disorder, or post-traumatic stress disorder (PTSD). The mind detaches from normal reasoning. It means that taking medication requiring complicated, closely timed dosing, while not impossible, can be close to it.
Drug and alcohol abuse scrambles the mind and reality—and here, too, adhering to a medication schedule becomes extremely difficult. Addiction to the abused substance further complicates the problem.
If you are living with HIV-infection, ARV non-compliance can have deadly consequences. Here are some tips to help make taking your meds easier:
Having HIV-infection is no longer a death sentence. But staying well requires medication, discipline and an understanding of the disease and how it’s treated. Talk to your provider if you have questions.
Leslie Vandever is a professional journalist and freelance writer with more than 25 years of experience. She lives in the foothills of Northern California where she writes for Healthline.
References:
• A Timeline of AIDD. (n.d.) AIDS.gov. U.S. Department of Health and Human Services. Retrieved on June 2, 2014 from http://aids.gov/hiv-aids-basics/hiv-aids-101/aids-timeline/
• About HIV/AIDS. (2014, Feb. 12) Centers for Disease Control and Prevention. Retrieved on June 3, 2014 from http://www.cdc.gov/hiv/basics/whatishiv.html
• Medication Adherence. (2009, Aug. 9) Aids.gov. U.S. Department of Health and Human Services. Retrieved on June 3, 2014 from http://aids.gov/hiv-aids-basics/just-diagnosed-with-hiv-aids/treatment-options/medication-adherence/
• Adherence. (n.d.) New Mexico AIDS Education and Training Center. National Library of Medicine. Retrieved on June 3, 2014 from http://www.aidsinfonet.org/fact_sheets/view/405
• White, J. M., et al. The Role of Substance Use and Mental Health Problems in Medication Adherence Among HIV-Infected MSM. (2014, June 6) LGBT Health. Retrieved on June 18, 2014 from http://online.liebertpub.com/doi/full/10.1089/lgbt.2014.0020
Your body’s tough. Its immune system produces protective T (thymus) cells to fight off infection by viruses, bacteria, and other foreign invaders from outside. Your T-cells step up and squash these malicious invaders before they can wreak havoc and make you sick.
But the human immunodeficiency virus, or HIV, specifically goes after and kills T-cells. In time, it kills off so many that there aren’t enough left to fight off the usual infections and diseases we’re all exposed to every day. The result is AIDS—acquired immunodeficiency syndrome.
When you have AIDS, you can get very sick, very quickly. Overcoming each illness requires monumental effort, and each battle leaves your body weaker. Eventually, one or more diseases or infections take over. Weakened and unable to fight back, you’ll die.
That’s the bleak truth about HIV/AIDS. But it doesn’t have to be that way.
So far, medical science hasn’t been able to find a cure for HIV, but antiretroviral treatments (ARVs) inhibit the virus in a number of ways, including its ability to reproduce. ARVs keep your “viral load” under control and your T-cells numerous enough to protect you from other viruses and diseases.
And that’s why it’s so important for you to take your HIV medications exactly as prescribed. Even a single missed dose can allow HIV to replicate and function better, making it that much harder for the ARV to bring it back under control. If you periodically skip doses or stop taking the medication temporarily, you’re setting your body up for AIDS.
Medication non-compliance is a well-known, widespread problem.
Missing medication doses or messing them up can happen to anyone, not just patients living with HIV-infection. Sometimes taking a dose is inconvenient—we’re not near a water source, or we’re otherwise occupied at the time we should be taking them and then forget to take them later. We’re all human. It happens.
Other reasons for ARV non-compliance are more complicated—and potentially more serious. According to a paper published in the peer-reviewed journal LGBT Health, mental health issues like depression, and substance abuse—particularly alcohol and crystal methamphetamine—are prevalent among gay, LGBT, bisexual and other men who have sex with men (MSM). They can have a profound and disastrous effect on an individual’s ability to stick to ARVs.
Just getting through each day can be a huge challenge if you’re suffering from depression, anxiety disorder, or post-traumatic stress disorder (PTSD). The mind detaches from normal reasoning. It means that taking medication requiring complicated, closely timed dosing, while not impossible, can be close to it.
Drug and alcohol abuse scrambles the mind and reality—and here, too, adhering to a medication schedule becomes extremely difficult. Addiction to the abused substance further complicates the problem.
If you are living with HIV-infection, ARV non-compliance can have deadly consequences. Here are some tips to help make taking your meds easier:
- Understand what you’re taking. Have your health care provider write down the names of your medications, what each of them looks like, and when and how often you need to take them. Keep this info handy for easy reference.
- Get pillboxes that hold a week’s worth of doses, divided into different times of the day (morning, noon, night, for instance). Fill them at the beginning of each week.
- Plan for changes in your regular routine, such as vacations or evenings out.
- Make sure you always have enough medicine. Refill bottles as soon as you’re able.
- Take your medicines at the same time each day to make taking them a habit.
- If your meds are causing side-effects that make it hard for you to take them, talk to your provider ASAP. They may be able to change the med or suggest ways to cope with the side-effect that helps you comply with dosing.
- If you’re experiencing mental health issues or abusing drugs or alcohol, seek help.
Having HIV-infection is no longer a death sentence. But staying well requires medication, discipline and an understanding of the disease and how it’s treated. Talk to your provider if you have questions.
Leslie Vandever is a professional journalist and freelance writer with more than 25 years of experience. She lives in the foothills of Northern California where she writes for Healthline.
References:
• A Timeline of AIDD. (n.d.) AIDS.gov. U.S. Department of Health and Human Services. Retrieved on June 2, 2014 from http://aids.gov/hiv-aids-basics/hiv-aids-101/aids-timeline/
• About HIV/AIDS. (2014, Feb. 12) Centers for Disease Control and Prevention. Retrieved on June 3, 2014 from http://www.cdc.gov/hiv/basics/whatishiv.html
• Medication Adherence. (2009, Aug. 9) Aids.gov. U.S. Department of Health and Human Services. Retrieved on June 3, 2014 from http://aids.gov/hiv-aids-basics/just-diagnosed-with-hiv-aids/treatment-options/medication-adherence/
• Adherence. (n.d.) New Mexico AIDS Education and Training Center. National Library of Medicine. Retrieved on June 3, 2014 from http://www.aidsinfonet.org/fact_sheets/view/405
• White, J. M., et al. The Role of Substance Use and Mental Health Problems in Medication Adherence Among HIV-Infected MSM. (2014, June 6) LGBT Health. Retrieved on June 18, 2014 from http://online.liebertpub.com/doi/full/10.1089/lgbt.2014.0020
Monday, June 2, 2014
Ordinary people doing extraordinary things...
It is that time again, when ordinary people are recognized for doing extraordinary things! On May 27th, a Call for Nominations was issued by the ADAP Advocacy Association for its 2014 Annual ADAP Leadership Awards. Now in its 4th year, these awards are designed to recognize individual, community, government and corporate leaders who are working to improve access to care and treatment under the AIDS Drug Assistance Programs (ADAPs).
This year's awards will be presented on Monday, August 5th during the ADAP Advocacy Association's 7th Annual Conference, being held at the Westin Washington City Center in Washington, DC. People living with HIV/AIDS have described the event has uplighting. Advocates have said the event reminded them of why they fight the good fight against the disease. There are some good laughs; there are definitely a lot of tears!
Bill Arnold, President & CEO of the Community Access National Network (CANN) and co-chair of the aaa+® board of directors said this about last year's event: “But one memorable highlight for many of us who have been doing this work for a long time was presenting former governor and HHS secretary Tommy Thompson with our Lifetime Achievement Award. His acceptance speech reminded everyone why we do this work for a living.”
Bill Arnold, President & CEO of the Community Access National Network (CANN) and co-chair of the aaa+® board of directors said this about last year's event: “But one memorable highlight for many of us who have been doing this work for a long time was presenting former governor and HHS secretary Tommy Thompson with our Lifetime Achievement Award. His acceptance speech reminded everyone why we do this work for a living.”
A Call for Nominations has been issued for the following awards:
- ADAP Champion of the Year (individual)
- ADAP Emerging Leader of the Year (individual)
- ADAP Corporate Partner of the Year
- ADAP Community Organization of the Year
- ADAP Lawmaker of the Year
- ADAP Social Media Campaign of the Year
- ADAP Grassroots Campaign of the Year
- ADAP Media Story of the Year
CLICK HERE to nominate a colleague, or submit a nomination to recognize an organization.
CLICK HERE to purchase a ticket to the awards dinner.
CLICK HERE to purchase a ticket to the awards dinner.
Friday, May 23, 2014
Patient Access Network Foundation – A Free Financial Resource for Underinsured Patients
By Amy Niles
Director of Patient Advocacy and Professional Relations, Patient Access Network (PAN) Foundation
For thousands of patients diagnosed with cancer and chronic illnesses, one of the first questions regarding their treatment and quality of life is, “How will I pay for this?” Patients who have been just getting by or even those who consider themselves fully financially stable often find themselves unable to afford the out-of-pocket costs associated with their prescribed medications. For many, the Patient Access Network (PAN) Foundation may be able to help.
Founded in 2004, the PAN Foundation is a nationwide, independent nonprofit dedicated to providing financial assistance to underinsured patients, or patients who have insurance but still face financial hardship in affording complex specialty medications. PAN has provided nearly $400 million in assistance to more than 250,000 patients across our nearly 60 disease-specific programs including a program for patients living with HIV/AIDS.
What is PAN assistance?
PAN provides grants to qualifying patients to help pay for the out-of-pocket portions of their qualifying medication costs. There is no cost to the patient or their healthcare provider to receive assistance from PAN. Once a patient is approved, PAN allocates a certain amount of money, $500-$10,000 varying by disease, that patients have access to for 12 months. When a patient receives a treatment or medication, their healthcare provider or specialty pharmacy submits a claim to PAN for the co-pay or coinsurance amount not covered by the patient’s insurance – allowing patients the peace of mind to continue their therapy without worrying about submitting reimbursement claims to PAN. PAN also features what we call a 90-day look-back, which means if a patient has incurred qualifying expenses at any time during the 90-days prior to their grant approval, PAN will reimburse them directly through their grant.
Who can qualify for PAN assistance?
PAN eligibility is often far more generous than most charity-care type programs, as we understand that the cost of specialty medications can be a burden even for those well above the poverty level. While criteria vary per disease-specific program, generally patients with household incomes at or below 400-500% of the federal poverty level ($62,920-78,650 for a family of two) are eligible to receive assistance. Patients must be insured and some programs require that patients have Medicare insurance. Patients must be diagnosed with one of the nearly 60 diseases for which PAN operates a program and must reside and receive treatment in the United States. Assistance is only available for mediations that treat the disease directly.
What assistance is available for patients living with HIV/AIDS?
Patients with HIV/AIDS can receive $4,000 per year to assist with the out-of-pocket costs associated with their medications. To qualify for assistance:
How to apply for PAN assistance:
PAN has developed multiple application routes, all delivering patients’ eligibility determinations in under one minute, so patients know instantly whether they have been approved for assistance.
To learn more about Patient Access Network and PAN’s assistance programs, visit www.PANfoundation.org.
Director of Patient Advocacy and Professional Relations, Patient Access Network (PAN) Foundation
For thousands of patients diagnosed with cancer and chronic illnesses, one of the first questions regarding their treatment and quality of life is, “How will I pay for this?” Patients who have been just getting by or even those who consider themselves fully financially stable often find themselves unable to afford the out-of-pocket costs associated with their prescribed medications. For many, the Patient Access Network (PAN) Foundation may be able to help.
Founded in 2004, the PAN Foundation is a nationwide, independent nonprofit dedicated to providing financial assistance to underinsured patients, or patients who have insurance but still face financial hardship in affording complex specialty medications. PAN has provided nearly $400 million in assistance to more than 250,000 patients across our nearly 60 disease-specific programs including a program for patients living with HIV/AIDS.
What is PAN assistance?
PAN provides grants to qualifying patients to help pay for the out-of-pocket portions of their qualifying medication costs. There is no cost to the patient or their healthcare provider to receive assistance from PAN. Once a patient is approved, PAN allocates a certain amount of money, $500-$10,000 varying by disease, that patients have access to for 12 months. When a patient receives a treatment or medication, their healthcare provider or specialty pharmacy submits a claim to PAN for the co-pay or coinsurance amount not covered by the patient’s insurance – allowing patients the peace of mind to continue their therapy without worrying about submitting reimbursement claims to PAN. PAN also features what we call a 90-day look-back, which means if a patient has incurred qualifying expenses at any time during the 90-days prior to their grant approval, PAN will reimburse them directly through their grant.
Who can qualify for PAN assistance?
PAN eligibility is often far more generous than most charity-care type programs, as we understand that the cost of specialty medications can be a burden even for those well above the poverty level. While criteria vary per disease-specific program, generally patients with household incomes at or below 400-500% of the federal poverty level ($62,920-78,650 for a family of two) are eligible to receive assistance. Patients must be insured and some programs require that patients have Medicare insurance. Patients must be diagnosed with one of the nearly 60 diseases for which PAN operates a program and must reside and receive treatment in the United States. Assistance is only available for mediations that treat the disease directly.
What assistance is available for patients living with HIV/AIDS?
Patients with HIV/AIDS can receive $4,000 per year to assist with the out-of-pocket costs associated with their medications. To qualify for assistance:
- A patient must be insured and insurance must cover the medication for which patient seeks assistance.
- A patient must reside and receive treatment in the U.S.
- The patient’s income must be at or below 500% of the Federal Poverty Level ($78,650 for a family of two).
How to apply for PAN assistance:
PAN has developed multiple application routes, all delivering patients’ eligibility determinations in under one minute, so patients know instantly whether they have been approved for assistance.
- To apply online, visit www.PANfoundation.org and select “Online Application.”
- To apply over the phone, call 866-316-PANF (7263). Representatives are available 9:00 am to 5:00 pm eastern time.
- Physicians and Specialty Pharmacists have access online portals where they may apply on behalf of patients and manage their grant and claims electronically.
To learn more about Patient Access Network and PAN’s assistance programs, visit www.PANfoundation.org.
Saturday, May 17, 2014
The Southern Epidemic
By Anna Meghan Nunn
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
The ADAP Advocacy Association (aaa+®) released an important White Paper on the impact of HIV/AIDS in the South, entitled “THE SOUTHERN EPIDEMIC: Are the South’s cultural, political and societal barriers making it difficult for public health programs, such as the AIDS Drug Assistance Programs, to function effectively in this region?” Its purpose is to examine why people living with HIV/AIDS in this region of the country often must overcome major obstacles simply to access basic healthcare needs, more so than any other area.
During “The Perfect Storm” — a label used by ADAP stakeholders to describe the severity of the AIDS Drug Assistance Program (ADAP) waiting list crisis that ravaged the program from 2008-2012 —nowhere in the U.S. was the HIV/AIDS crisis more apparent than the South. At any given moment in the crisis, nearly 95% of the people living with HIV/AIDS being denied access to care and treatment resided in the South. At the height of the ADAP crisis, eight of the twelve states that instituted waiting lists were in the South; most of them in the Deep South.
The Center for Disease Control and Prevention (CDC) estimates that there are approximately 1,144,500 people aged 13 years and older living with HIV infection in the U.S. today. The southeastern United States has seen a disproportionate impact of HIV/AIDS in their communities, especially over the last decade. In 2011, eight of the southern states accounted for the ten states with the highest new HIV infections in the country. Furthermore, southeastern states accounted for 50% of HIV infections that year. To put that in perspective, it is important to note that this region accounts for only 37% of the U.S. population. There are numerous contributing factors behind these alarming numbers. This region of the country has historically been known to have retained a deep and distressing culture, evidenced by violent civil rights struggles, high poverty rates, poor education systems, deeply engrained religious traditions, and limited access to healthcare.
In the South many societal, economic, and geographic constraints collide to create a “Perfect Storm,” which ultimately creates barriers to healthcare. Some of these factors include:
• Race and discrimination
• Poverty and education
• Sexual orientation and stigma
The complex dynamics of these factors not only impact access to adequate healthcare, but create a great deal of stress for State ADAPs in this region. By race African Americans are the largest group affected by HIV/AIDS. In fact, in 2010 new HIV infection rates among African Americans were 8 times that of whites. This is a trend we are beginning to see within the Latino community as well. The South is also home to a large amount of individuals living in poverty. In addition, this region typically has below average literacy levels. Both poverty and poor education are associated with lower access to healthcare and negative health outcomes. An additional cultural factor weighing on HIV/AIDS infection rates in the South is the Evangelical attitudes and traditional conservative values associated with the religious South. These traditional conservative values regarding sexual orientation can foster a climate of stigma and shame toward the largest group of people living with HIV/AIDS: men who have sex with men (MSM). These societal and cultural factors in the southern states combine to create barriers to health care.
Access to Healthcare
Societal factors are only a part of the complex issue regarding the disproportionate rates of HIV/AIDS infections in the South. The lack of access to healthcare is also a major contributing factor this crisis in the South.
This leaves many people living with HIV/AIDS in the South only two options for health care: Medicaid and the Ryan White CARE Act programs like state ADAPs. Unfortunately, it is still too early to tell how the Affordable Care Act (ACA) will play out in the months or years to come with regard to this population. While the ACA has afforded many the opportunity to gain insurance coverage through Marketplace Exchange programs, many low-income people living with HIV/AIDS are falling into Medicaid gaps. This is a result of the southern states’ rejection of federal funding to expand Medicaid eligibility to more citizens. With the exception of Arkansas, all of the “Deep South” states have made the decision not to expand their Medicaid coverage.
This leaves thousands of people living with HIV/AIDS to rely on Ryan White services like ADAPs for health care coverage. However, there is cause for concern as southern states have historically been less than generous in the amount of voluntary funds they provide to their state ADAPs. For example, nationally states contribute an estimated 14% to the total ADAP budget. However, southern states have typically contribute lower than average or not at all. Arkansas, Louisiana, Mississippi, and Kentucky have never contributed any state funds to the ADAP programs. In 2009 South Carolina contributed 11% and Florida contributed only 9%. The recent economic recession and subsequent rises in unemployment rates has increased the demand for ADAP services. Unfortunately the recession also has resulted in deeper budget cuts in southern states. The state of North Carolina saw their ADAP budget cut by $8 million in the fiscal years 2014-15.
These imminent budget cuts have forced state ADAPs to initiate cost-containing measures like enrollment caps and reduced formularies. The unfortunate unintended consequences of these cost-containing measures is the looming threat of national ADAP waiting lists, something the programs have been successful at reducing and nearly eliminating in recent years.
CLICK HERE to download the White Paper: “THE SOUTHERN EPIDEMIC: Are the South’s cultural, political and societal barriers making it difficult for public health programs, such as the AIDS Drug Assistance Programs, to function effectively in this region?”
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
The ADAP Advocacy Association (aaa+®) released an important White Paper on the impact of HIV/AIDS in the South, entitled “THE SOUTHERN EPIDEMIC: Are the South’s cultural, political and societal barriers making it difficult for public health programs, such as the AIDS Drug Assistance Programs, to function effectively in this region?” Its purpose is to examine why people living with HIV/AIDS in this region of the country often must overcome major obstacles simply to access basic healthcare needs, more so than any other area.
During “The Perfect Storm” — a label used by ADAP stakeholders to describe the severity of the AIDS Drug Assistance Program (ADAP) waiting list crisis that ravaged the program from 2008-2012 —nowhere in the U.S. was the HIV/AIDS crisis more apparent than the South. At any given moment in the crisis, nearly 95% of the people living with HIV/AIDS being denied access to care and treatment resided in the South. At the height of the ADAP crisis, eight of the twelve states that instituted waiting lists were in the South; most of them in the Deep South.
The Center for Disease Control and Prevention (CDC) estimates that there are approximately 1,144,500 people aged 13 years and older living with HIV infection in the U.S. today. The southeastern United States has seen a disproportionate impact of HIV/AIDS in their communities, especially over the last decade. In 2011, eight of the southern states accounted for the ten states with the highest new HIV infections in the country. Furthermore, southeastern states accounted for 50% of HIV infections that year. To put that in perspective, it is important to note that this region accounts for only 37% of the U.S. population. There are numerous contributing factors behind these alarming numbers. This region of the country has historically been known to have retained a deep and distressing culture, evidenced by violent civil rights struggles, high poverty rates, poor education systems, deeply engrained religious traditions, and limited access to healthcare.
In the South many societal, economic, and geographic constraints collide to create a “Perfect Storm,” which ultimately creates barriers to healthcare. Some of these factors include:
• Race and discrimination
• Poverty and education
• Sexual orientation and stigma
The complex dynamics of these factors not only impact access to adequate healthcare, but create a great deal of stress for State ADAPs in this region. By race African Americans are the largest group affected by HIV/AIDS. In fact, in 2010 new HIV infection rates among African Americans were 8 times that of whites. This is a trend we are beginning to see within the Latino community as well. The South is also home to a large amount of individuals living in poverty. In addition, this region typically has below average literacy levels. Both poverty and poor education are associated with lower access to healthcare and negative health outcomes. An additional cultural factor weighing on HIV/AIDS infection rates in the South is the Evangelical attitudes and traditional conservative values associated with the religious South. These traditional conservative values regarding sexual orientation can foster a climate of stigma and shame toward the largest group of people living with HIV/AIDS: men who have sex with men (MSM). These societal and cultural factors in the southern states combine to create barriers to health care.
Access to Healthcare
Societal factors are only a part of the complex issue regarding the disproportionate rates of HIV/AIDS infections in the South. The lack of access to healthcare is also a major contributing factor this crisis in the South.
This leaves many people living with HIV/AIDS in the South only two options for health care: Medicaid and the Ryan White CARE Act programs like state ADAPs. Unfortunately, it is still too early to tell how the Affordable Care Act (ACA) will play out in the months or years to come with regard to this population. While the ACA has afforded many the opportunity to gain insurance coverage through Marketplace Exchange programs, many low-income people living with HIV/AIDS are falling into Medicaid gaps. This is a result of the southern states’ rejection of federal funding to expand Medicaid eligibility to more citizens. With the exception of Arkansas, all of the “Deep South” states have made the decision not to expand their Medicaid coverage.
This leaves thousands of people living with HIV/AIDS to rely on Ryan White services like ADAPs for health care coverage. However, there is cause for concern as southern states have historically been less than generous in the amount of voluntary funds they provide to their state ADAPs. For example, nationally states contribute an estimated 14% to the total ADAP budget. However, southern states have typically contribute lower than average or not at all. Arkansas, Louisiana, Mississippi, and Kentucky have never contributed any state funds to the ADAP programs. In 2009 South Carolina contributed 11% and Florida contributed only 9%. The recent economic recession and subsequent rises in unemployment rates has increased the demand for ADAP services. Unfortunately the recession also has resulted in deeper budget cuts in southern states. The state of North Carolina saw their ADAP budget cut by $8 million in the fiscal years 2014-15.
These imminent budget cuts have forced state ADAPs to initiate cost-containing measures like enrollment caps and reduced formularies. The unfortunate unintended consequences of these cost-containing measures is the looming threat of national ADAP waiting lists, something the programs have been successful at reducing and nearly eliminating in recent years.
CLICK HERE to download the White Paper: “THE SOUTHERN EPIDEMIC: Are the South’s cultural, political and societal barriers making it difficult for public health programs, such as the AIDS Drug Assistance Programs, to function effectively in this region?”
Friday, April 25, 2014
When the Rubber (ACA) Hits the Road (ADAP)
By Anna Meghan Nunn
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
The ADAP Advocacy Association, in conjunction with the Community Access National Network's Hepatitis: Education, Advocacy & Leadership (HEAL) project, held their fourth annual summit in Washington D.C. last week. The event entitled, "The Intersection Between the ACA and ADAP," was held on Monday, April 14th - Tuesday, April 15th, 2014. The summit's purpose was to “assemble stakeholders to discuss the Affordable Care Act as it relates to individuals living with HIV/AIDS and individuals living with Viral Hepatitis, especially the law’s impact on services and supports funded under the AIDS Drug Assistance Program.”
The summit was open to the public and included a variety of stakeholders from the public health, advocacy, medical, pharmaceutical and government sectors, as well as numerous patients currently receiving services under the AIDS Drug Assistance Program (ADAP). Thirty invited panelists attended, eight of which gave presentations that focused on current issues and enduring questions within the HIV/AIDS community. The presentations included:
Michael Shankle, with HealthHIV, facilitated the discussion, guiding participants through the lengthy and thoughtful conversations that helped make the summit a success. He opened the summit by asking each panelist to use one word to describe the ACA/ADAP intersection; he used the responses to generate a word cloud.
The summit kicked off with an overview from Emily McCloskey, NASTAD. The presentation addressed the following points:
Matt Salo, National Association of Medicaid Directors, gave the next presentation which addressed the issues surrounding Medicaid Eligibility Expansion and the ACA. Key points from this discussion included:
Next, Jeff Crowley, Georgetown Law's O’Neill Institute for National and Global Health Law, focused on how the ACA has expanded the role of ADAPs as insurance providers. Main points that were brought up in the discussion included the following:
The afternoon began with presentations from Glen Pietrandoni, Walgreens, and Joey Wynn, , Empower U. These presentations dealt with issues related to wrap-around services in the Marketplace exchange. The discussion yielded the following points:
Scott Schoettes, Lambda Legal, followed with an update on the lawsuit against Blue Cross Blue Shield (BCBS) of Louisiana. His engaging presentation followed up on an emerging issue previously reported in February 2014. The issue involves a case by Lambda Legal in response to the discriminatory practices by BCBS of Louisiana in which the insurance company denied third-party payments, including Ryan White grantees. Schoettes’ presentation provided background information on this case, as well as information regarding the outcome. As it stands now, BCBS of Louisiana has agreed to continue accepting third-party payments from Ryan White funds through the end of the calendar year. The Centers for Medicare and Medicaid Services (CMS), in the meantime, issued a final interim rule mandating that the insurance giant reverse their policy. Schoettes’ presentation was enlightening and became a catalyst for great discussions about the need to stay vigilant against discriminatory practices in how the ACA is applied moving forward.
A. Toni Young, Community Education Group discussed the need for appropriate care for people living with HIV/AIDS who are transitioning back into the community after incarceration. Young’s presentation focused on the need for HIV testing in the lower-income areas of Washington D.C. She made a point to note that most infections happen in the community rather than in penitentiaries and jails. She stressed the importance of helping individuals gain access to healthcare upon release. Her agency's progressive plans include empowering these individuals to re-enter their communities, take control of their healthcare, and assist in HIV testing in their neighborhoods.
The final presentation of the day was delivered by Daniel Raymond, Harm Reduction Coalition, on the comorbidity of HIV, Hepatitis C, and substance abuse. The talk focused on leveraging ACA and ADAP to address these co-occurring issues. Key points that arose during the discussion include:
There was serious concern expressed over the Obama Administration’s proposal to merge Ryan White’s Part C and Part D, as well as the premature introduction of legislation to reauthorize the law. At the center of the concern over Ryan White reauthorization is funding may be on the chopping block in the future as a result of the implementation of the ACA. The general consensus among the group was that Ryan White funds are still very critical to affording healthcare, medications, and wraparound services. Everyone in attendance agreed that we must remain cautious and keep a watchful eye on this matter as the ACA rollout continues.
In closing, panelists agreed on the following:
Interested in a patient's perspective on the summit? Go to HEAL blog, "ADAP Summit on the Intersection Between ACA & ADAP"
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
The ADAP Advocacy Association, in conjunction with the Community Access National Network's Hepatitis: Education, Advocacy & Leadership (HEAL) project, held their fourth annual summit in Washington D.C. last week. The event entitled, "The Intersection Between the ACA and ADAP," was held on Monday, April 14th - Tuesday, April 15th, 2014. The summit's purpose was to “assemble stakeholders to discuss the Affordable Care Act as it relates to individuals living with HIV/AIDS and individuals living with Viral Hepatitis, especially the law’s impact on services and supports funded under the AIDS Drug Assistance Program.”
The summit was open to the public and included a variety of stakeholders from the public health, advocacy, medical, pharmaceutical and government sectors, as well as numerous patients currently receiving services under the AIDS Drug Assistance Program (ADAP). Thirty invited panelists attended, eight of which gave presentations that focused on current issues and enduring questions within the HIV/AIDS community. The presentations included:
- “A Year of Change: ADAP’s Successes and Challenges Implementing the Affordable Care Act”— Emily McCloskey, Manager, Policy and Legislative Affairs, National Alliance of State & Territorial AIDS Director (NASTAD)
- “Update on ACA Medicaid Expansion”— Matt Salo, Executive Director, National Association of Medicaid Directors
- “The Continuing Role of ADAPs as Health Insurance Coverage is Expanded by the Affordable Care Act”— Jeff Crowley, Program Director, National HIV/AIDS Initiative, Georgetown Law, O’Neill Institute for National and Global Health Law
- “ADAPs & Wrap Around Services in Marketplace Plans”— Glen Pietrandoni, Senior Director, Pharmacy Services, Walgreens & Joey Wynn, Community Relations Director, Empower U
- “Update on Blue Cross Blue Shield of Louisiana & Discriminatory Marketplace Exchange Practices”— Scott Schoettes, HIV Project Director, Lambda Legal
- “Mind the Gap: Ensuring Appropriate Care for Incarcerated Patients Transitioning Back Into Their Communities”— A. Toni Young, Executive Director, Community Education Group
- “Co-occurring Challenges: Leveraging ADAP and ACA to Address Hepatitis C and Substance Abuse Disorders”— Daniel Raymond, Policy Director, Harm Reduction Coalition
Michael Shankle, with HealthHIV, facilitated the discussion, guiding participants through the lengthy and thoughtful conversations that helped make the summit a success. He opened the summit by asking each panelist to use one word to describe the ACA/ADAP intersection; he used the responses to generate a word cloud.
The summit kicked off with an overview from Emily McCloskey, NASTAD. The presentation addressed the following points:
- Medical Homes
- Treatment incentives
- ADAP co-pays
- Drugs
- Drug co-pays Possible elimination of combo drugs
- HRSA- Purchasing insurance must match ADAP formulary
Matt Salo, National Association of Medicaid Directors, gave the next presentation which addressed the issues surrounding Medicaid Eligibility Expansion and the ACA. Key points from this discussion included:
- State Strategies
- In need of tools
- Patient vs. Politics
- Politics wins as state Medicaid directors are often forced to tow the line of their Governor’s agenda
- Risk pools increase cost
- Young and healthy are not enrolling
- Private option more expensive
- Medicaid does not factor in risk pools
- Private--> marketplace--> diversifies risk pool
- Need 400% FPL enrollment
- Do substitutions make plans more affordable 100% FPL to 133% FPL
- Supportive Services
- Medicaid staff with HIV-specific experience decreased
- States deliver the most medications to the most people
- Leveraging resources
- Sub-optimal therapies
- Cheapest isn’t always best
- Essential role of community providers
- Continuity of care
Next, Jeff Crowley, Georgetown Law's O’Neill Institute for National and Global Health Law, focused on how the ACA has expanded the role of ADAPs as insurance providers. Main points that were brought up in the discussion included the following:
- Focus on individuals
- Falling through the cracks
- Need to provide education about available plans
- Need to educate providers
- Collecting better data
- Healthcare reform is about integration
- How do we thoughtfully distribute the funding
- How to educate new leaders
- Develop "champions"
- Treatment as prevention
- Reauthorization needs to address funding (e.g., formulas)
- Fairness (where located)
- Must have community input
- Equity equals decreased competence
- Emergency focus and examination
- Non-expansion states increased disparities
- Need to create a balance between incentives and punishment of states
- Difficult conversations are necessary
- People respond to success
- Broaden coalitions
- Nurture younger voices
- More consumer engagement
- Responsibility of consumers
- Agency engagement
- Consumer drive
The afternoon began with presentations from Glen Pietrandoni, Walgreens, and Joey Wynn, , Empower U. These presentations dealt with issues related to wrap-around services in the Marketplace exchange. The discussion yielded the following points:
- Expand role providers and pharmacists
- Tools need to be developed using local assumptions and factors
- Help consumers pick plans with models and make informed decisions
- How states make payments
- Streamline process
- Provider needs on plan
- Not always plan but office manager/system barriers
- State by state breakdown in medications
- Programs negotiate pricing based on contracts
- Rebates vary
Scott Schoettes, Lambda Legal, followed with an update on the lawsuit against Blue Cross Blue Shield (BCBS) of Louisiana. His engaging presentation followed up on an emerging issue previously reported in February 2014. The issue involves a case by Lambda Legal in response to the discriminatory practices by BCBS of Louisiana in which the insurance company denied third-party payments, including Ryan White grantees. Schoettes’ presentation provided background information on this case, as well as information regarding the outcome. As it stands now, BCBS of Louisiana has agreed to continue accepting third-party payments from Ryan White funds through the end of the calendar year. The Centers for Medicare and Medicaid Services (CMS), in the meantime, issued a final interim rule mandating that the insurance giant reverse their policy. Schoettes’ presentation was enlightening and became a catalyst for great discussions about the need to stay vigilant against discriminatory practices in how the ACA is applied moving forward.
A. Toni Young, Community Education Group discussed the need for appropriate care for people living with HIV/AIDS who are transitioning back into the community after incarceration. Young’s presentation focused on the need for HIV testing in the lower-income areas of Washington D.C. She made a point to note that most infections happen in the community rather than in penitentiaries and jails. She stressed the importance of helping individuals gain access to healthcare upon release. Her agency's progressive plans include empowering these individuals to re-enter their communities, take control of their healthcare, and assist in HIV testing in their neighborhoods.
The final presentation of the day was delivered by Daniel Raymond, Harm Reduction Coalition, on the comorbidity of HIV, Hepatitis C, and substance abuse. The talk focused on leveraging ACA and ADAP to address these co-occurring issues. Key points that arose during the discussion include:
- AIDS still leading cause of death for people living with HIV/AIDS
- Co-infection treatment is coming
- New drugs may be less complex than other older drugs (and more expensive)
- Drug rebates unclear
- Re-infection and treatment rates
- Identify who should be tested/treated
- Completion of treatment is difficult (8 days to 2 weeks)
- HCV treatment is usually not emergency
- Adherence assessment
- Public health impact
- Waiting for states to determine Medicaid benefit for HCV treatment
- Guidelines from national partners drive change and increase access
- Need for a structured formalized platform to discuss future of the Ryan White law
- Model to assess formulary, out of pocket cost, provider network
- Minimize formulary STND needed for ADAP
- Access of social media in reaching target population
- Follow up and more collaboration on discriminatory practices
There was serious concern expressed over the Obama Administration’s proposal to merge Ryan White’s Part C and Part D, as well as the premature introduction of legislation to reauthorize the law. At the center of the concern over Ryan White reauthorization is funding may be on the chopping block in the future as a result of the implementation of the ACA. The general consensus among the group was that Ryan White funds are still very critical to affording healthcare, medications, and wraparound services. Everyone in attendance agreed that we must remain cautious and keep a watchful eye on this matter as the ACA rollout continues.
In closing, panelists agreed on the following:
- Need for more centralized, aggregated data
- Fresh faces and new blood- innovative and new ideas
- More holistic patient perspectives
- More access to information
- Community consensus around Ryan White is necessary to keep the funding
- Collaboration and not duplication
- Increases in engagement and volunteering
Interested in a patient's perspective on the summit? Go to HEAL blog, "ADAP Summit on the Intersection Between ACA & ADAP"
Thursday, April 10, 2014
United Healthcare Does 180 Degree on Mail Order Pharmacy
By Anna Meghan Nunn
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
A lawsuit filed in June 2013 by Consumer Watchdog and
handled by national law firm Whatley Kallas, LLC
in Orange County federal court has reached a settlement, bringing welcome news to many United Healthcare policy holders living with HIV/AIDS. The class action
lawsuit was filed against the nation’s largest health insurance company. In the lawsuit, Consumer Watchdog alleged that the insurance giant was
illegally forcing its policy holders living with HIV/AIDS to order their prescription medications
through their own in-house mail-order pharmacy. When United Healthcare made the decision, these policy holders were forced to make a choice: transfer their prescriptions
to its in-house mail-order pharmacy or pay thousands of dollars out of pocket
to continue their relationships with their local retail pharmacists.
 The settlement was reached on March 20, 2014; it required United Healthcare to
allow patients to opt-out of the mail-order plan and resume receiving their
medications at their local pharmacy.
The settlement was reached on March 20, 2014; it required United Healthcare to
allow patients to opt-out of the mail-order plan and resume receiving their
medications at their local pharmacy.
Intern from the University of North Carolina at Wilmington, Department of Public and International Affairs
In June 2013, PR Newswire published an article, quoting Consumer Watchdog staff attorney Jerry Flanagan as saying:
“United’s decision to
force their most vulnerable members into a pharmacy program not of their
choosing is harmful to the very people United is supposed to be protecting.
Patients, not insurers, should be allowed to decide how, when and where they buy
their medications.”
The argument against the mail-order plan is four fold.
First, healthcare advocates fear that eliminating the
patient-pharmacist relationship would have adverse effects on the patient’s
ability to navigate the complications that come with taking multiple medications
as part of a daily routine. Pharmacists are unable to monitor potential drug
interactions when they are cut out of the healthcare process through the
implementation of mail-order plans. Additionally, pharmacists offer valuable
counseling and advice that many patients depend on.
Pharmacists are in a unique position to assist patients with
questions they may have about their medications before they take them home.
Further, they are able to develop relationships with patients that further
assist with ensuring safe and proper adherence to their prescription drug
routines. As it stands now, United has replaced these relationships with an 800
number.
A second concern about these mail-order plans is that they
cause patients to miss out on discounts offered exclusively at retail
pharmacies. In a time when rising costs of medications is increasingly
burdening people living with HIV/AIDS, these opportunities to save money on
medications are crucial.
A further reservation is that there is a serious issue of
patient-privacy with mail-order plans. A news release
issued by Consumer Watchdog (3/20/2014) clarifies this point stating, “…HIV/AIDS specialty
medications often are delivered in refrigerated containers. Patients who live
in apartment buildings or have medications delivered to their work-place have
expressed alarm that neighbors, co-workers, and employees, who do not know that
the recipient has HIV/AIDS, would come to suspect that they are seriously ill.”
Finally, there is the issue of time lag with mail delivery. Many of
these medications must be refrigerated and therefore are time sensitive. In
addition, these medications are often life-saving for some of the most vulnerable
people living with HIV/AIDS. The issue of time lag with respect to slow
delivery, mix-ups at the postal service, and mishandling of medications could
potentially be life threatening.
Consumer Watchdog had also alleged that United
Healthcare’s requirement was discriminatory in nature, illegally targeting
those policy holders living with HIV/AIDS.
The ADAP Advocacy Association agreed. In a press release
issued last year in response to another insurance carrier mandating the same policy to its policy holders living with HIV/AIDS, Brandon Macsata said:
“Patients should be
afforded as many treatment options as possible, especially when combating a
chronic disease such as HIV/AIDS. Any policy that restricts the patient’s
ability to interact directly with healthcare professionals, including a
pharmacist, is counter intuitive to promoting better medication adherence,
which is critically important to improved health.”
Although this statement was in response to another lawsuit filed by
Consumer Watchdog against Anthem Blue Cross of California, its message rings
true in this case as well.
Consumer Watchdog settled a similar lawsuit against Anthem Blue Cross
of California in May 2013. The difference between that lawsuit and this one is
that the Anthem Blue Cross case only impacted clients in the state of
California whereas this settlement will apply to, “…individual
and employer-provided health plans across the country, and allows patients the
right to exercise their opt-out right for a broader range of medications by
written opt-out, United’s website,
and over the phone” (Consumer Watchdog
3/20/2014).
The court is expected to finish its review in July 2014. They will then
notify Class members of their decision and allow the opt-out process to begin.
Additionally, Class members who paid more for their prescriptions due to the
mail-order plan may seek reimbursement for those costs.
The ADAP Advocacy Association welcomes the news of this
settlement with United Healthcare. The reversal of United Healthcare’s decision brings less
complication for patients, increased knowledge of medications, and more
productive relationships between patients and their healthcare professionals.